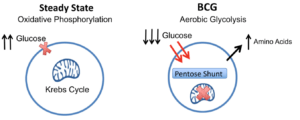
BCG treatment switches cellular metabolism from oxidative phosphorylation to early aerobic glycolysis: The systemic lowering of blood sugars in T1Ds after BCG vaccines combined with the increased glucose uptake and purine synthesis is consistent with BCG switching cellular metabolism to early aerobic glycolysis. This hypothesis holds that BCG causes downregulation of the Krebs cycle, accelerated aerobic glycolysis, increased glucose uptake, and shunting of glucose to the Pentose Phosphate Shunt for augmented purine biosynthesis. Source Figure 3c: Kühtreiber et al., 2018.
Bacillus Calmette–Guérin (BCG) vaccine developed to protect individuals from developing tuberculosis (TB), is known to be associated with reduced morbidity and mortality due to other-non-TB illnesses. In fact it is used for bladder cancer therapy. This has led to research that aims at determining other beneficial uses of BCG against both communicable and non-communicable diseases. An example of such research, is the use of BCG as a diabetic therapeutic agent.
Mouse models of Type 1 diabetes have demonstrated a beneficial effect of repeated BCG vaccination against diabetes. BCG vaccination in mice has been shown to prevent development of autoimmune diabetes, and in some cases even reverse advanced diabetes. Thus, researchers from Boston (Massachusetts General Hospital and Harvard, USA) investigated the potential long term benefits of BCG (2 doses) vaccination on Type 1 diabetes in adults.
Researchers conducted a phase 1 clinical trial where individuals were either vaccinated with two doses of BCG or placebo two weeks apart, followed by the standard of care type 1 diabetes treatment. Researchers observed a decrease in hemoglobin A1c (HbA1c) to near normal levels in BCG vaccinated individuals after 3 years post vaccination. These low (near normal) levels of HbA1c were sustained in BCG vaccinated individuals for a further 5 years (end of follow up).
Surprisingly, researchers showed that improved blood sugar control observed in BCG vaccinated individuals was neither due to an increase in pancreatic insulin -as observed in the murine model- nor peripheral insulin resistance. Instead, blood sugar control was associated with an improvement of glucose metabolism. Where BCG vaccination favoured aerobic glycolysis over oxidative phosphorylation, this resulted in increased breakdown of glucose to produce amino acids (via the pentose phosphate shunt). Additionally, using mouse models researchers showed that BCG-induced aerobic glycolysis is able to prevent treatment induce hyperglycemia in mice.
Overall, this study demonstrates the potential utility of BCG as a cheap and safe therapeutic agent against type 1 diabetes. A finding that still needs to be validated on a larger cohort, and in tuberculosis endemic areas where BCG is currently given.
Journal Article: Kühtreiber et al., 2018. Long-term reduction in hyperglycemia in advanced type 1 diabetes: the value of induced aerobic glycolysis with BCG Vaccinations. Vaccines npj
Article by Cheleka AM Mpande.










