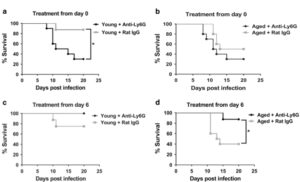
Fig.1 Neutrophil depletion at the end of the first week p.i. (postinfection) enhances survival in aged mice. a Young mouse were administered a neutrophil-depleting monoclonal antibody just prior to inoculation with influenza virus and following infection (as described in Materials and methods) and survival was monitored. Compared to isotype control treated mice, neutrophil-depleted young mice exhibited a significant increase in mortality. *P < 0.05 (Log rank), n = 8–10 per group. b Aged mice were treated per a and survival postinfection was monitored. P value between neutrophil-depleted and control group, P=0.23 (Log-Rank). n=8–10 per group. c Young mice were administered a neutrophil-depleting antibody at day +6 p.i., then intermittently until day +12 p.i. (as described in Materials and methods) and compared to isotype control treated, young infected mice. *P = 0.10 (Log-rank), n = 8–10 per group. d Aged mice were treated according to c and survival was measured postinfection. Aged neutrophil-depleted mice exhibited a significant increased survival as compared to the control group. *P < 0.05 Log-rank, n = 8–10 per group
Influenza virus infection causes more mortality in elderly compared to younger people, and one of the main reasons could be aging of the immune system. Aging impairs both innate and adaptive immune responses, compromising the immune response to influenza virus infection.
During influenza virus infection (flu) in the lung, neutrophils are recruited and help in viral infection clearance through phagocytosing of viral particles, producing extracellular traps and activating inflammasome. Macrophages remove neutrophils to prevent excessive neutrophil function after a viral infection. People >60 years exhibit impaired neutrophil function; however, it is not clear how aging affects neutrophil function during flu which was the objective of the study conducted by Kulkarni et al., using a murine model.
Aged mice infected with influenza showed a 3-fold increase in neutrophils count in the lung compared to young mice 6 days post-infection. Depletion of neutrophils after Influenza infection, improves survival of aged mice to 80% from 40% in controls, while it did not impact viral clearance (Fig1). However, depletion of neutrophils at the onset of viral infection exacerbates the survival rate leading to increased mortality. These findings suggest that excessive neutrophil recruitment and function are responsible for mortality in aged mice. Neutrophils isolated from bone marrow of aged mice showed increased chemotaxis towards bronchoalveolar lavage (BAL) collected from aged mice compared to young mice. Consistent with these results, levels of neutrophil chemoattractant, i.e., CXCL1 and CXCL2 in the BAL showed a 2-4-fold increase in comparison to young mice and antibody-blockade of CXCL1 and CXCL2, reduced the neutrophil chemotaxis towards aged lung lysate. To investigate the source of chemo-attractants, alveolar epithelial cells (AECs) were isolated and cultured from young and aged mice. AECs from aged mice produced the highest levels of CXCL1 and CXCL2.
Overall, these findings indicate that the mechanism by which excessive neutrophils accumulation occurs after Influenza virus infection is through AEC produced CXCL1 and CXCL2 recruitment of neutrophils. This study implies that mortality in older people infected with the influenza virus could be reduced by therapies that target AECs, neutrophils, and interactions between AECs and neutrophils.
Journal article: Kulkarni et al., 2019 Excessive neutrophil levels in the lung underlie the age-associated increase in influenza mortality. Mucosal Immunology (2019) 12:545–554
Article by Avid Mohammadi











