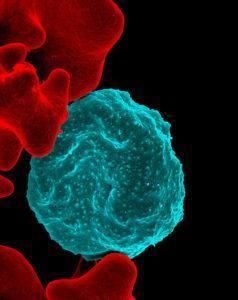
Colorized scanning electron micrograph of red blood cell infected with malaria parasites (NIAID, Wikimedia Commons)
BCG is one of the first vaccines to be given to infants. Epidemiological studies have shown a protective effect of BCG against non-related infections, where BCG vaccination is associated with reduced infant mortality. Recent studies hypothesise that improved outcomes is due to BCG trained immunity, where BCG primes innate immune cells to confer a non-specific resistance to infection. In humans, one study has shown that BCG vaccination reduces viremia in individual vaccinated with live attenuated yellow fever vaccine (Arts et al., read our summary). However, there is limited research on the impact of BCG on malaria. Murine models have shown that BCG reduces parasitaemia in mice compared to controls. Researchers aimed to provide evidence of the protective effect of BCG on malaria outcomes in humans.
Walk et al., showed that BCG vaccination didn’t lead to lower levels of parasitaemia post malaria challenge (controlled human malaria infection) compared to controls. However, BCG vaccinees developed clinical symptoms faster and had a higher frequency of symptoms and adverse events compared to controls. BCG has been shown to prime and activate innate immune cells. In theory this increased activation would enable rapid innate immune responses to microorganisms reducing replication rate and pathology. At 7 days post CHMI (blood stage) researchers observed higher proportion of activated (CD69+) NK and gd T cells in BCG vaccinees. Correlation analysis of clinical symptoms and immune profiles, showed that activation of NK cells (CD69+) and monocytes (HLA-DR+) was associated with lower parasitaemia in BCG vaccinees but not controls. Indicating a potential role of NK cells and monocyte in BCG-mediated trained immunity against malaria. Despite not observing higher proportions of adaptive immune responses in BCG vaccinees compared to controls, during CHMI. Researchers showed that BCG-vaccinees had significantly higher proportions of granzyme B expressing NK cells and CD4+ T cells compared with controls.
In summary, this study suggests that trained immunity induced by BCG vaccination, particularly activation of NK cells and monocytes, is associated with lower parasitaemia. However, the study was under-powered to demonstrate significant difference in other immunological outcomes measured. Unfortunately, the study was designed to treat individuals as soon as parasitaemia was observed, thus researchers could not demonstrate the effect of BCG vaccination on self-resolving malaria immunity.
Journal Article: Walk et al., 2019. Outcomes of controlled human malaria infection after BCG vaccination. Nature Communications.
Article by Cheleka AM Mpande











