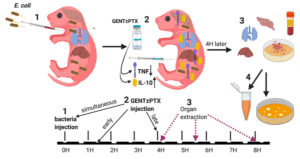
Experimental design. (1) Neonatal mice (< 24 h old) were injected with E. coli via the right intra-jugular route at the start of the experiment (0H time point). (2) Subsequently, pups were injected intraperitoneally with GENT, PTX, (GENT + PTX), or saline control immediately following bacteria injection (simultaneously, at the 0H time point), early (1.5H after bacteria injection), or late (4H after bacteria injection). (3) After additional 4H of incubation, i.e., at the 4H, 5.5H, or 8H time point from the start of the experiment, mice were euthanized and blood and organs obtained for (4) bacterial plating and cytokine measurements. (Source: Speer et al., 2020)
Sepsis is a life-threatening disease caused by a dysregulated immune response that induces systemic and organ dysfunction. Infants are responsible for almost 50% of all sepsis cases, majority of whom are under 5 years old (World Health Organisation: Sepsis Fact Sheet). Treatment of neonatal sepsis is very challenging, with many neonates either dying or developing neurological-developmental disability. Pentoxifylline (PTX) is a candidate neonatal sepsis immunotherapy, however, due to limitations in trial design and implementation, its efficacy has not been demonstrated. Fortunately, animal models: S. aureus induced sepsis in mice& group B streptococci associated sepsis in rabbits have demonstrated the ability of PTX to contribute to clearance of the pathogen and decrease inflammation. In humans, most sepsis cases in neonates are due to infection with Escherichia coli, thus Speer et al., tested Pentoxifylline (PTX), Gentamycin* or combination of the two to treat neonatal (E.coli) sepsis in mice. Their research built on previous work that showed that PTX played a role in reducing bacterial burden using an in vitro model on (E.coli infection of cord-blood).
Using the E.coli neonatal sepsis model they demonstrated dissemination of E.coli to other parts of the body including the brain was also associated with detection of detrimental sepsis-associated inflammatory cytokines. They showed that PTX modestly decreased TNF levels, but significantly increased levels of the anti-inflammatory cytokine IL-10 without creating an environment for bacterial proliferation. GTX on the other hand, reduced levels of IL-1b, thus in combination with PTX performed very well in reducing hyperinflammatory associated pathology. Researchers concluded that “[their] study demonstrated that adjunctive PTX when added to GENT, inhibited E. coli-induced TNF and enhanced E. coli-induced IL-10 production in blood plasma while also increasing anti-inflammatory IL-10 concentrations in peripheral organ tissues including the brain.”
*Gentamycin is a broad spectrum antibiotic
Journal Article: Speer et al., 2020. A Neonatal Murine Escherichia coli Sepsis Model Demonstrates That Adjunctive Pentoxifylline Enhances the Ratio of Anti- vs. Pro-inflammatory Cytokines in Blood and Organ Tissues. Frontiers in Immunology
Summary by Cheleka Mpande










