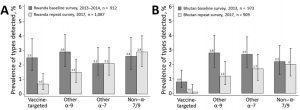
Overall crude human papillomavirus prevalence by general primer GP5+/6+-mediated PCR in baseline and repeat surveys in Rwanda (A) and Bhutan (B), with corresponding 95% CIs. Vaccine-targeted types (HPV-6, -11, -16, -18); other α-9 types (HPV-31, -33, -35, -52, -58); other α-7 types (HPV-39, -45, -59, -68); non–α 7/9 types (HPV-26, -51, -53, -56, -66, -70, -73, -82).
Cervical cancer is the fourth most commonly diagnosed type of cancer in women globally and the first or second in low- and middle-income countries (LMICs). There were 604,000 cervical cancer cases and 342,000 deaths in 2020 globally with Sub-Saharan Africa bearing the highest burden.1 Vaccination has successfully been used to save millions of lives that could otherwise be lost to various infectious diseases. Most vaccines developed to date train our immune system to protect the body against foreign pathogens. HPV infection is attributable to about 99.7% of cervical cancer cases globally in addition to other anogenital and oropharyngeal cancers. Development of cancer vaccines is a sophisticated process due to the fact that there are no clear single foreign pathogens attributable to most known cancers, hence the current intensive focus on development of therapeutic cancer vaccines. However, given that cancer cells are self-cells that have undergone unregulated cell growth and the immune system is naturally trained not to recognize self-antigens, most therapeutic vaccines have not been effective enough and have been dropped at early trial phases.
There are currently three licenced HPV vaccines: Cervarix (Bivalent HPV 16/18), Gardasil (quadrivalent HPV 6/11/16/18) and Gardasil 9 (HPV 6/11/16/18/31/33/45/52/58) all with clearly demonstrated excellent efficacy and immunogenicity against the main potent and carcinogenic HPV types and related diseases and or cancers. Despite its potential for cervical cancer elimination 2 HPV vaccination coverage is very low especially in LMICs where factors such as lack of awareness, early screening and treatment programs contribute to the highest cervical cancer burden. This has been due to various social, cultural and economic reasons that discourage vaccine uptake.
Rwanda and Bhutan were among the first LMICs to introduce HPV vaccination at national levels in 2011 and 2010, respectively, achieving over 90% uptake in females 12-18 years old.
Iacopo Baussano and colleagues have recently published data from these two countries which is the first to demonstrate HPV vaccine effectiveness in LMICs. 3 They assessed the impact of Catch-up HPV vaccination by comparing prevalence of HPV infection in women aged 17–22 years in successive urine-based surveys conducted in high schools during 2013–2014 (baseline survey) and 2017 (repeat survey) in both countries. DNA was extracted from urine samples and tested for vaccine and non-vaccine HPV genotypes using PCR assay. They reported an overall effectiveness against Gardasil vaccine-targeted HPV types HPV 6/11/16/18 to be 78% (95% CI 51%–90%) in Rwanda, and 88% (6%–99%) in Bhutan and against other alpha-9 genus HPV types to be 58% in Rwanda and 63% in Bhutan, suggesting cross-protection. They did not detect vaccine effect against other HPV types tested. The prevalence of vaccine-targeted and the 9 additional cross-protected HPV types decreased significantly.
Despite study limitations acknowledged by the authors, these findings provide direct evidence from LMICs of the marked effectiveness of high-coverage school-based, national HPV vaccination programs.
This sets a good example to be emulated by other countries in efforts to eliminate cervical cancer in the region. National HPV vaccination has been implemented in a number of countries where it has reduced the prevalence of vaccine targeted HPV types and prevented related diseases significantly.
Despite current global health challenges in health systems among them immunization programs due to the current COVID-19 pandemic, it is paramount for governments to put in place measures that ensure national vaccination programs are implemented and new vaccines continue to be introduced.
Journal Articles
- Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians
- Brisson, M. et al. Impact of HPV vaccination and cervical screening on cervical cancer elimination: a comparative modelling analysis in 78 low-income and lower-middle-income countries. The Lancet 395, 575-590, doi:10.1016/S0140-6736(20)30068-4 (2020).
- Baussano, I. et al. Impact of Human Papillomavirus Vaccination, Rwanda and Bhutan. Emerg Infect Dis 27, 1-9, doi:10.3201/eid2701.191364 (2021).
Summary by Eunice Kiambi










