Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) where the immune system mistakenly attacks the lining of the colon. Current medications help many patients, but some remain unresponsive. This suggests existing treatments might not fully target the culprit immune cells driving the inflammation.
Recent research has shed light on a new potential target for treating UC: stem-like T cells (Figure 1). These T cells, a type of white blood cell, act like cellular reservoirs, continuously producing more immune cells that fuel inflammation.
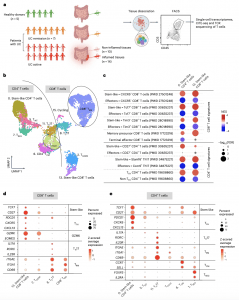
Figure 1: Stem-like CD4+ and CD8+ T cells were found in colonic tissue. a, Study overview. b, Single-cell transcriptomes of colonic T cells from healthy controls and patients with UC displayed by uniform manifold approximation and projection (UMAP). Seurat-based clustering of 13,887 T cells, colored based on cluster type; labels indicate assigned T cell subset cluster identity. c, GSEA plot shows enrichment of the indicated gene signatures (Supplementary Table 3) obtained from the sources shown. False discovery rate (FDR) and normalized enrichment score (NES) were determined using fgsea package on R. d, Plot shows Z-score average expression (color scale) and percentage of cells (size scale) that expressed selected marker gene transcripts that were significantly enriched (FDR ≤ 0.05) in the indicated cluster when compared to the other colonic CD8+ T cells. e, Similar plots for CD4+ T cells.
Scientists compared colonic tissue samples from UC patients with healthy controls. They found higher levels of stem-like T cells, particularly cytotoxic T cells (CD8+) and helper T cells (CD4+), in inflamed areas of UC patients’ colons. This suggests these cells play a role in initiating and maintaining inflammation.
Further analysis revealed a close genetic link between stem-like T cells and other inflammatory T cell populations in UC patients. This suggests stem-like T cells might be responsible for the persistence of these harmful immune cells.
To test this theory, researchers used a specialized mouse model of UC. They found that CD4+ helper T cells lacking specific genes (BCL-6 and TCF1) crucial for stem cell function were less pathogenic (disease-causing). This implies that targeting stemness in T cells might be a viable therapeutic strategy.
This study provides strong evidence for the involvement of stem-like T cells in UC. Targeting these cells could lead to the development of new and more effective treatments for UC patients who currently have limited options.
Journal article: Li, Y., et al., 2024. Stem-like T cells are associated with the pathogenesis of ulcerative colitis in humans. Nature Immunology.
Summary by Stefan Botha










