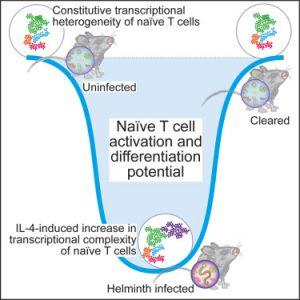
The immune system is an intricate and highly regulated network that protects the body from pathogens while avoiding damage to self-tissues. A cornerstone of this system is the balance between immune activation and tolerance, with naive CD4+ T cells playing a crucial role in orchestrating these responses. The article titled “The Amalgam of Naive CD4+ T Cell Tolerance and Autoimmunity” offers an in-depth exploration of how naive CD4+ T cells maintain immune tolerance and how their dysregulation can lead to autoimmune diseases (Figure 1).
Naive CD4+ T cells are a subset of T cells that have not yet encountered their specific antigen. They circulate through the blood and lymphoid tissues, waiting to be activated by antigen-presenting cells (APCs). The activation of these cells is a critical event in the immune response, as it determines whether the immune system will respond aggressively to an antigen or maintain tolerance. The article elaborates on the essential processes governing this decision, focusing on how the immune system avoids attacking self-antigens—a concept central to the prevention of autoimmunity.
A major aspect discussed in the article is the process of thymic selection, which is vital for developing a self-tolerant T cell repertoire. During their development in the thymus, T cells undergo both positive and negative selection. Positive selection ensures that T cells can recognize self-major histocompatibility complex (MHC) molecules, while negative selection eliminates T cells that react too strongly to self-antigens. However, not all self-reactive T cells are deleted; some escape into the periphery, where additional mechanisms of tolerance are required to prevent autoimmune reactions.
Peripheral tolerance is another key concept addressed in the article. This mechanism involves several strategies to prevent autoimmunity, including anergy (a state of unresponsiveness), deletion (cell death), and regulation by T regulatory (Treg) cells. Treg cells are particularly important in maintaining peripheral tolerance. They function by suppressing the activation and proliferation of potentially autoreactive T cells, thereby preventing immune responses against self-tissues. The article discusses the various cytokines and signalling pathways involved in the development and function of Treg cells, emphasising their role in immune homeostasis.
The breakdown of these tolerance mechanisms is a significant contributor to the development of autoimmune diseases. The article explores various factors that can lead to this breakdown, including genetic predispositions, environmental triggers, and infections. For instance, genetic mutations in key immune regulatory genes can impair Treg cell function, leading to uncontrolled T cell activation and autoimmunity. Environmental factors, such as exposure to certain chemicals or drugs, can also disrupt immune tolerance by altering the function of naive CD4+ T cells or Treg cells. Infections can trigger autoimmune responses through mechanisms such as molecular mimicry, where the immune system mistakenly targets self-antigens that resemble pathogen antigens.
A detailed analysis of molecular signalling pathways is provided in the article, particularly those that regulate naive CD4+ T cell activation and differentiation. Key signalling molecules, such as cytokines and co-stimulatory receptors, play critical roles in determining the fate of these cells. For example, the interaction between CD28 on T cells and B7 molecules on APCs provides a crucial co-stimulatory signal necessary for full T cell activation. The article also highlights the role of specific cytokines, such as interleukin-2 (IL-2), in promoting the proliferation and differentiation of naive CD4+ T cells into various effector subsets, including Th1, Th2, Th17, and Treg cells. Each of these subsets has distinct functions in the immune response, with Th1 cells involved in cell-mediated immunity, Th2 cells in humoral immunity, Th17 cells in inflammation, and Tregs in immune suppression.
The article also delves into the role of epigenetic modifications in regulating the function of naive CD4+ T cells. Epigenetic changes, such as DNA methylation and histone modification, can influence the expression of genes involved in T cell activation, differentiation, and tolerance. These modifications can be inherited or induced by environmental factors, adding a layer of complexity to immune regulation. The article discusses how dysregulation of these epigenetic mechanisms can lead to inappropriate immune responses and autoimmunity. For instance, alterations in the methylation status of genes encoding key regulatory proteins can result in the loss of Treg cell function and the development of autoimmune diseases.
The relationship between naive CD4+ T cells and the microbiome is another important area explored in the article. The gut microbiota, consisting of trillions of commensal microorganisms, plays a significant role in shaping the immune system, including the development and function of naive CD4+ T cells. The article highlights how the microbiota influences the immune system’s ability to distinguish between self and non-self, promoting immune tolerance while preventing inappropriate immune activation.
One of the key insights discussed is the role of specific microbial communities in regulating immune responses. Certain commensal bacteria are known to promote the differentiation of naive CD4+ T cells into regulatory T cells (Tregs), which are crucial for maintaining immune tolerance. These bacteria produce metabolites, such as short-chain fatty acids (SCFAs), that influence the epigenetic landscape of T cells, promoting a regulatory phenotype. Disruptions to the microbiome, such as those caused by antibiotics, diet, or infections, can lead to a loss of this regulatory influence, resulting in immune dysregulation and increased susceptibility to autoimmune diseases.
Furthermore, the article discusses how the microbiome can impact systemic immunity. While much of the immune system’s interaction with the microbiota occurs in the gut, the effects of this interaction are not confined to the gastrointestinal tract. Signals generated by the microbiota can influence immune responses throughout the body, affecting the function of naive CD4+ T cells in various tissues. For example, the article notes that changes in the composition of the gut microbiota can alter the balance between pro-inflammatory and regulatory T cell responses, potentially leading to autoimmune inflammation in distant organs such as the skin, joints, and central nervous system.
The article also addresses the concept of “mucosal tolerance,” a mechanism by which the immune system maintains tolerance to antigens encountered at mucosal surfaces, such as those of the gut, lungs, and urogenital tract. Naive CD4+ T cells are exposed to a variety of antigens at these surfaces, including dietary antigens, commensal bacteria, and inhaled particles. Mucosal tolerance is essential for preventing inappropriate immune responses to these antigens, which could otherwise lead to chronic inflammation and tissue damage. The article explores the mechanisms underlying mucosal tolerance, including the role of dendritic cells, which present antigens to naive CD4+ T cells in a way that promotes tolerance rather than activation.
In the context of autoimmune diseases, the article provides a detailed discussion of how failures in these tolerance mechanisms can lead to pathogenesis. For example, in diseases such as inflammatory bowel disease (IBD), a breakdown in mucosal tolerance leads to uncontrolled immune responses against gut microbiota, resulting in chronic inflammation. Similarly, in multiple sclerosis, the failure to maintain tolerance to self-antigens in the central nervous system leads to an immune attack on myelin, the protective sheath surrounding nerve fibres. The article underscores the importance of understanding these mechanisms to develop targeted therapies that restore tolerance and prevent autoimmune disease progression.
Finally, the article touches on the therapeutic potential of manipulating naive CD4+ T cells and their regulatory networks to treat autoimmune diseases. One promising approach is the use of biologics, such as monoclonal antibodies, to modulate cytokine signalling pathways involved in T cell activation and differentiation. Another strategy involves the use of small molecules or gene-editing techniques to alter the epigenetic landscape of T cells, promoting a regulatory phenotype that can suppress autoimmune responses. Additionally, the article discusses the potential of microbiome-based therapies, such as probiotics or faecal microbiota transplantation, to restore a healthy microbiome and re-establish immune tolerance.
In conclusion, “The Amalgam of Naive CD4+ T Cell Tolerance and Autoimmunity” provides a comprehensive overview of the complex mechanisms by which naive CD4+ T cells maintain immune tolerance and how their dysregulation can lead to autoimmune diseases. The article emphasises the importance of understanding the factors that regulate T cell activation, differentiation, and tolerance to develop new therapeutic strategies for autoimmune conditions. By highlighting the roles of thymic selection, peripheral tolerance, molecular signalling pathways, epigenetic modifications, and the microbiome, the article offers valuable insights into the intricate balance between immune defence and tolerance, and the consequences of its disruption.
Journal article: Even, Z., et al., 2024. The amalgam of naive CD4+ T cell transcriptional states is reconfigured by helminth infection to dampen the amplitude of the immune response . Cell Immunity.
Summary by Faith Oluwamakinde