Introduction Hematocrit, an essential indicator of blood health, is significantly affected in patients co-infected with HIV and malaria. This review delves into how co-infection impacts hematocrit levels, complicating disease progression and clinical outcomes in endemic regions.
Take a look into how far we have come: Reflecting on AIDS 2016
In HIV patients, hematocrit fluctuations are common due to anemia induced by immune dysregulation and opportunistic infections. Antiretroviral therapy (ART) improves hematocrit levels by suppressing viral load and reducing inflammation; however, certain ART drugs may negatively affect bone marrow function.
Malaria infection leads to a drop in hematocrit due to red blood cell destruction by Plasmodium parasites. Severe malaria cases show marked decreases in hematocrit, indicative of anemia. Hematocrit recovery post-treatment reflects effective parasite clearance and red blood cell restoration.
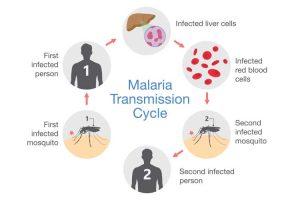
Figure 1: When female Anopheles mosquitoes feed on blood to nurture their eggs, they can pick up Plasmodium parasites from humans infected with malaria. These mosquitoes will then become vectors (carriers) and transmit Plasmodium to other people they bite. You can not contract malaria directly from another person (CDC 2022).
The combined effects of HIV and malaria further reduce hematocrit, intensifying anemia in co-infected individuals. Immune modulation, including increased cytokine release, exacerbates red blood cell destruction. Monitoring hematocrit levels in co-infected patients provides insights into disease severity and guides treatment.
Regular hematocrit monitoring is crucial for managing anemia in HIV-malaria co-infection. Addressing hematocrit fluctuations through targeted therapies, including ART and antimalarial drugs, can help mitigate complications and improve outcomes. Preventative measures, such as malaria prophylaxis, are essential for at-risk populations.
Hematocrit levels serve as a vital indicator in co-infected patients, where fluctuations reflect the impact of both infections. A multidisciplinary approach integrating ART, antimalarial therapies, and hematocrit monitoring is recommended to manage the complex dynamics of HIV-malaria co-infection.
Journal article: Obeagu EI, Okwuanaso CB, Edoho SH, Obeagu GU. Under-nutrition among HIV-exposed Uninfected Children: A Review of African Perspective. Madonna University Journal of Medicine and Health Sciences. 2022; 2(3):120-127.
Summary by Faith Oluwamakinde










