A comprehensive narrative review on emergency contraception (EC), published in the European Journal of Obstetrics and Gynaecology, provides a detailed overview of the different methods available for preventing pregnancy after unprotected sex. Emergency contraception is a critical tool in reducing unintended pregnancies, and the review explores the mechanisms, efficacy, and clinical considerations of the most commonly used EC methods: levonorgestrel (LNG), ulipristal acetate (UA), and the copper intrauterine device (IUD).
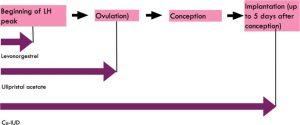
The review emphasizes that all forms of emergency contraception work by delaying or inhibiting ovulation, preventing fertilization before it can occur. Levonorgestrel is a progestin-only pill that is most effective when taken within 72 hours of unprotected intercourse. Ulipristal acetate, a progesterone receptor modulator, can be used up to 120 hours (five days) after unprotected intercourse and offers a slightly longer window of efficacy compared to levonorgestrel. The copper IUD is the most effective form of EC, with a near 100% success rate when inserted within five days after intercourse. Unlike the oral methods, which only delay ovulation, the copper IUD also prevents fertilization by creating an inhospitable environment for sperm.
The review discusses the safety profiles of these methods, noting that LNG and UA are both well-tolerated, with the most common side effects being mild and transient, such as headaches, nausea, and changes in menstrual patterns. The copper IUD, though highly effective, carries a small risk of uterine perforation and may cause heavier menstrual bleeding in some women. However, its long-term contraceptive benefits, which can last up to 10 years, make it an attractive option for women seeking both emergency and ongoing contraception.
The article also highlights the challenges in accessing emergency contraception, particularly in low-resource settings or countries where EC is restricted. In many parts of the world, women face significant barriers to obtaining EC, including lack of availability, cost, and the requirement of a prescription for certain methods. The review calls for increased access to EC, particularly for vulnerable populations, as a means of reducing unintended pregnancies and the subsequent need for abortions.
In addition, the review notes that despite its availability, many women are not fully informed about EC options or how to use them effectively. Misconceptions about EC, including the mistaken belief that it causes abortion, contribute to its underuse. The article emphasizes the importance of educating both healthcare providers and patients about the mechanisms and correct use of EC to ensure that it is used effectively when needed.
In conclusion, the review underscores the critical role that emergency contraception plays in reproductive healthcare. By offering multiple methods with varying windows of efficacy, EC provides women with options for preventing pregnancy after unprotected sex. However, to maximize the public health benefits of EC, it is essential to improve access, reduce stigma, and increase awareness about how and when to use these methods.
Journal article: Mierzejewska, Anna, et al. “Emergency Contraception – a Narrative Review of Literature.” European Journal of Obstetrics & Gynecology and Reproductive Biology, vol. 299, 13 June 2024, pp. 188–192, https://doi.org/10.1016/j.ejogrb.2024.06.015.
Summary by Faith Oluwamakinde