Stroke is a major health concern, with effects that extend beyond the brain. A recent study published in Nature Medicine reveals how brain injuries trigger long-term changes in immune responses that contribute to cardiac dysfunction. Researchers identified a process known as innate immune memory in which monocytes and macrophages become “primed” by IL-1β after stroke, leading to persistent inflammation and damage to the heart.
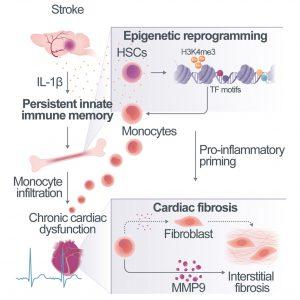
Figure 1: Acute brain ischemia leads to persistent innate immune memory, innate immune memory causes chronic post-stroke cardiac dysfunction
The study used both human stroke patients and animal models to investigate how brain injury leads to prolonged immune activation. The researchers focused on how brain injuries create a state of heightened responsiveness in monocytes and macrophages. Following the initial stroke event, these immune cells maintain an exaggerated inflammatory response due to their “memory” of the brain injury, even after the brain begins to recover. This phenomenon was termed “innate immune memory” and was found to drive chronic inflammation in the heart.
IL-1β was identified as a critical molecule in this process, perpetuating the heightened inflammatory state in immune cells. The prolonged immune response contributes to cardiac dysfunction, characterized by fibrosis and reduced heart function. Notably, blocking IL-1β signalling or preventing monocyte trafficking to the heart significantly reduced heart damage, suggesting a potential therapeutic avenue for post-stroke care.
Implications for Treatment
This study’s findings open up new opportunities for therapeutic intervention. Current stroke management focuses on the brain, but these results suggest that addressing immune changes could prevent longer-term complications, particularly those affecting the heart. By targeting IL-1β or preventing immune cell migration to the heart, there may be new ways to protect stroke survivors from chronic cardiac conditions. This could be especially important in reducing mortality and improving the quality of life for stroke survivors.
Innate immune memory offers a new understanding of how brain injuries can have lasting impacts on other organs. This study highlights the potential of immune-targeted therapies, specifically IL-1β inhibitors, in preventing cardiac dysfunction following stroke. Further research is needed to translate these findings into clinical practice, but they represent a promising step forward in holistic stroke care.
Journal Article: Simats, Alba, et al. “Innate Immune Memory after Brain Injury Drives Inflammatory Cardiac Dysfunction.” Cell.
Summary by Faith Oluwamakinde










