Giant cell arteritis (GCA) and polymyalgia rheumatica (PMR) are inflammatory conditions that affect older individuals, often causing significant morbidity. Until recently, treatment approaches for these conditions varied widely, leading to inconsistent outcomes. A 2024 study published in Annals of the Rheumatic Diseases outlines the first treat-to-target (T2T) recommendations for GCA and PMR, providing a structured approach to achieving better patient outcomes through individualized treatment plans.
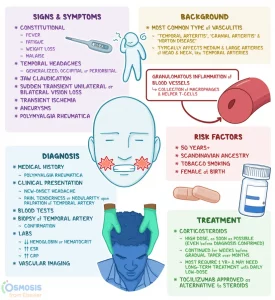
Figure 1: Giant cell arteritis (GCA) and polymyalgia rheumatica (PMR) are overlapping inflammatory rheumatic conditions of older people.
Why Treat-to-Target?
Treat-to-target (T2T) is a widely adopted concept in rheumatology that involves setting specific treatment goals, regularly monitoring progress, and adjusting treatment as needed to achieve and maintain remission. The 2024 T2T guidelines for GCA and PMR were developed by an international task force of experts who reviewed existing literature and combined evidence with expert opinion. The aim is to maximize health-related quality of life, prevent complications, and reduce the side effects associated with treatments like glucocorticoids (GCs), which are the cornerstone of therapy for both diseases.
Key Recommendations
The guidelines set forth five overarching principles and six specific recommendations. The primary goal of treatment for both GCA and PMR is to achieve and maintain remission, which is defined as the absence of clinical symptoms and systemic inflammation. In GCA, preventing tissue ischemia and vascular damage is also a critical goal, given the risk of blindness and other complications. Regular monitoring is essential, especially during GC tapering, to ensure that remission is maintained without excessive use of medication.
GCs remain the primary treatment for both conditions, but the guidelines emphasize the importance of minimizing GC-related side effects. For patients with more severe disease or a high risk of relapse, adjunct therapies like tocilizumab (TCZ) may be considered, especially in GCA. Methotrexate is another option, though its effectiveness is less clear. The task force also highlighted the need for shared decision-making between patients and healthcare providers to tailor treatment based on individual needs and comorbidities.
Challenges and Future Directions
One of the challenges in managing GCA and PMR is balancing the need for aggressive treatment to control inflammation with the risk of long-term side effects from medications like GCs. Up to 60% of patients experience relapses, which can lead to further complications. Additionally, rapid GC tapering, as seen in clinical trials, may not be feasible in real-world settings, highlighting the need for individualized tapering schedules.
The guidelines also identify several gaps in the current understanding of GCA and PMR. For example, while imaging techniques like ultrasound can detect vascular inflammation, their role in routine monitoring remains unclear. Future research should focus on defining remission more precisely, investigating biomarkers for early diagnosis, and exploring new treatment options that can reduce reliance on GCs.
The treat-to-target approach offers a promising framework for improving the management of GCA and PMR. By setting clear treatment goals, regularly monitoring disease activity, and adjusting therapies based on individual patient needs, clinicians can better control these chronic conditions and minimize treatment-related complications. As more data becomes available, these guidelines will likely evolve, offering even more refined strategies for managing GCA and PMR.
Journal Article: Dejaco, Christian, et al. “Treat-To-Target Recommendations in Giant Cell Arteritis and Polymyalgia Rheumatica.” Annals of the Rheumatic Diseases.
Summary by Faith Oluwamakinde










