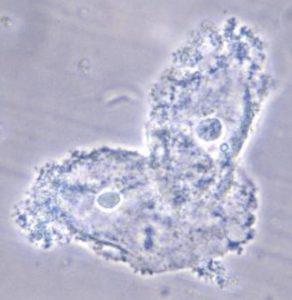
The female reproductive tract (FRT) has numerous physiological and immunological barriers against HIV infection. In addition to being a physical barrier, FRT epithelial cells possess toll-like receptors (TLR) that illicit of innate cytokines and mediators in response to vaginal and pathogenic microbiota.
Microbial metabolites have been observed to modulate gut immunity. However, little is known about the immunomodulatory effects microbial metabolites have on the FRT. Women with a “normal” Lactobacillus spp dominated microbiota have reduced susceptibility to HIV and sexually transmitted infection (STIs) than women with vaginal dysbiosis such as bacteria vaginosis. Lactic acid represents a major microbial metabolite present in “normal” vagina microbiota, contrastingly the level of this metabolite is greatly decreased in women with bacterial vaginosis. The increased risk of HIV and STIs acquisition in bacterial vaginosis affected women has been shown to be associated with increased levels of pro-inflammatory cytokines, a response to vaginal microbiota dysbiosis, which results in recruitment of HIV target CD4+ T cells.
Hearps et al. aimed to determine the immunomodulatory effects of lactic acid on FRT epithelial cells, as well as its effect on immune responses induced to microbial pathogen associated molecular patterns (PAMPs) and seminal plasma.
Hearps et al. demonstrated that lactic acid independently decreases production of pro-inflammatory mediator IL-6 and increases production of anti-inflammatory cytokine IL-1 receptor agonist (IL-1RA) by FRT epithelial cells exposed to 0.3% lactic acid in transwell cultures. Additionally, lactic acid is able to inhibit inflammatory responses induced by TLR agonists LPS, Pam3C and polyinosinic–polycytidylic acid by significantly decreasing production of IL-6, IL-8, TNF-a, RANTES and MIP3-a, and increasing production of IL-1RA. The immunomodulatory effect of lactic acid on FRT epithelial cells exposed to TLR agonists was not solely mediated by low pH, demonstrated by no immunomodulatory effect of low pH (without lactic acid) on pro-inflammatory cytokines induced by the TLR agonists. Finally, Hearps et al demonstrated that lactic acid is capable of dampening seminal plasma induced production of pro-inflammatory cytokine IL-8 by FRT epithelial cells.
In summary, Hearps et al. illustrated an immunomodulatory role of lactic acid, a major microbial metabolite of “normal” vagina microbiota that dampens pro-inflammatory responses and induces production of anti-inflammatory cytokine, IL-1RA. Females are eight time more likely to acquire HIV following vaginal intercourse than their male counterparts.The data generated by Hearps et al. illustrates a role of lactic acid in reduction of FRT immune activation, that can be harnessed in future topical microbicides that aim to prevent HIV acquisition.
Journal Article: Hearps et al. 2017. Vaginal lactic acid elicits an anti-inflammatory response from human cervicovaginal epithelial cells and inhibits production of pro-inflammatory mediators associated with HIV acquisition. Mucosal Immunology
Article by Cheleka AM Mpande