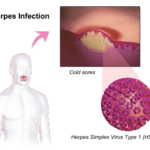
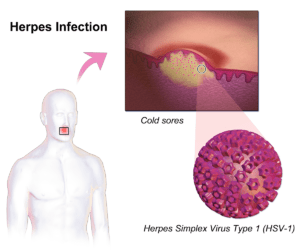
Herpes is a life long infection caused by either herpes simplex virus type 1 (HSV-1) or type 2 (HSV-2), with an estimated worldwide prevalence of 67% and 11%, respectively. HSV-1 predominantly causes oral herpes (cold sores) but can also cause genital herpes, a sexually transmitted infection, whereas HSV-2 primarily causes genital herpes. There is currently no cure for Herpes, however therapeutics that alleviate symptoms are available.
Studies of herpes suggest that successful control of virus is associated with robust CD8 T cells responses. Thus, it is not surprising, that tested HSV vaccine candidates that successfully induce humoral immunity have had limited success. This highlighs the need for further research that aims at determining mechanisms that regulate recruitment of CD8 T cells to vaginal mucosal tissues during HSV-infection. CXCL17 is one of the most highly expressed mucosal associated chemokines which has been shown to have homeostatic and inflammatory properties.
Srivastava et al., aimed to determine if CXCL17 is essential for recruiting antiviral CXCR8+ CD8+ T cells, and whether these cells contribute to protective immunity against genital herpes. Researchers used a murine (C57BL/6) model of HSV-1 infection to determine protective HSV-1 immune responses in wild type and CXCL17 knock-out (KO)mice. Researchers showed that protective HSV-1 immunity was associated with increased production of CXCL17 compared to non-protected mice. High levels of CXCL17 was associated with increased proportions of functional cytotoxic-IFN-γ expressing effector (TEM) and tissue resident (TRM) CXCR8+ CD8 T cells at the vaginal mucosal, main site of infection. Additionally, Srivastava et al., also demonstrated that HSV-1-specific CD8 T cells induced by HSV-1 infection in CXCL17 KO mice were less functional and expressed exhaustion markers such as TIGIT. This was associated with increased pathology and reduced frequencies of CXCR8+ TEM and TRM CD8+ T cells.
Development of an HSV vaccine is one of the strategies to combat the spread of HSV infections. This research could inform future vaccine strategies that could leverage the CXCL17-CXCR8 pathway, that has been shown to be important for the induction and recruitment of protective HSV-1 specific responses to the vaginal mucosal.
* CXCR8 is the CXCL17 chemokine receptor.
Journal Article: Srivastava et al., 2018. CXCL17 Chemokine−Dependent Mobilization of CXCR8 +CD8+ Effector Memory and Tissue-Resident Memory T Cells in the Vaginal Mucosa Is Associated with Protection against Genital Herpes. Journal of Immunology
Article by Cheleka AM Mpande