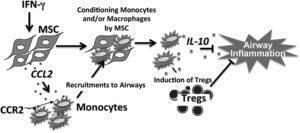
Proposed model for IFN-γ activation, CCL2 production, and monocyte recruitment in MSC-mediated suppression of AHR and airway inflammation. (Source: Takeda et al., 2018. Journal of Immunology)
Asthma is one of the most common respiratory diseases. In spite of improvements in treating asthma, treatment of severe asthma remain a challenge. One of the many avenues being explored for the treatment of severe asthma is the use of mesenchymal stem cells (MSCs).
MSCs, also known as stromal cells, are multipotent cells that have the ability to differentiate into specialised cell types. MSCs can be isolated from many adult tissues, though the most efficient MSCs are derived from bone marrow. MSCs have been shown to have immunomodulatory properties, including the ability to induce production of immunoregulatory cytokines TGFβ and IL-10, as well as activation of regulatory T cells and monocytes/macrophages. Clinically MSCs have been shown to suppress immune responses during inflammatory diseases such as Inflammatory Bowel Diseases.
Current research has shown that administration of MSCs is associated with reduced symptoms during severe asthma. Takeda et al., aimed to determine interactions between MSCs and monocytes during an experimental model of allergen-induced airway inflammation in C57BL/6 mice that lead to reduced symptoms.
Researches showed that administration of MSCs before or after allergen challenge resulted in reduction of air hyper responsiveness and eosinophilia in lung bronchoalveolar lavage fluid. However, administration of MSCs prior to allergen challenge selectively resulted in reduced levels of Th2 cytokines (IL-4, IL-5 and IL-13) and significant increase in IL-10 in lung bronchoalveolar lavage fluid compared to control mice. Thus confirming that during an an experimental allergen challenge model MSCs do suppress airway inflammation. This MSC-induced suppression of airway inflammation was dependent on the presence of monocytes suggestion interaction between MSCs and monocytes.
Using various knock out mice, researchers clearly showed that MSCs are require IFNg to induce secretion of the chemokine CCL2, which results in the recruitment of monocytes via the chemokine CCR2. These recruited monocytes are then activated to secrete IL-10 which leads to reduced airway inflammation and hyper responsiveness.
Journal Article: Takeda et al., 2018. Mesenchymal Stem Cells Recruit CCR2+ Monocytes To Suppress Allergic Airway Inflammation. Journal of Immunology.
Article by Cheleka AM Mpande











