The RV144 or Thai Trial conducted in Thailand, is the only HIV vaccine trial to date that has demonstrated modest efficacy, 60.5% efficacy up to 12 months after vaccination. Analysis of results from the RV144 HIV vaccine trial showed that high levels of HIV Envelope protein (Env)-specific IgA antibodies correlated with increased risk of HIV infection. However, evidence from non-human primate simian immunodeficiency virus (SIV) challenge models suggests that SIV-specific IgA can result in reduced HIV acquisition at mucosal sites. Wills et al., aimed to determine if human HIV-specific IgA antibodies induced by RV144 vaccine can mediate antiviral activity in vitro.
Researchers isolated two IgA monoclonal antibodies (MAb), HG129 and HG130, from memory B cell cultures of peripheral blood from HIV-uninfected RV144 vaccinees. Characterisation of antibody binding specificity demonstrated that HG130 bound to various gp120 vaccine strain antigens, illustrating that HG130 was indeed a vaccine induced antibody. Unlike HG130, HG129 weakly bound to any vaccine strain antigens, suggesting that HG129 was likely an HIV Env cross-reactive clone that was not directly elicited by vaccination.
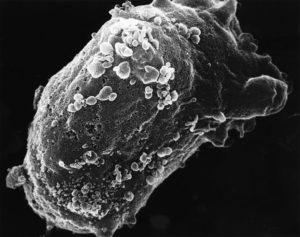
Analysis of HIV-specific IgA responses suggested that increased risk of HIV acquisition could be attributed to Env-specific IgA competing with IgG-mediated antibody mediated cellular cytotoxicity (ADCC). Researches showed that HG129 and HG130 IgA MAbs were unlikely to interfere with IgG-mediated ADCC because HG129 and HG130 were unable to bind to HIV infected cells nor neutralize HIV in vitro cell cultures.
Galacotsylceramide (Galcer) is an alternative receptor HIV-1 receptor that allows HIV to infect cells that do not express CD4 receptor, such as epithelial cells. Researchers demonstrated that HG129 but GH130 was able to block HIV-1 1086.C strain gp140 Env glycoprotein binding to Galcer. Thus HG129 could be a potential candidate for blocking binding of virus to epithelial lining at mucosal sites.
Finally, the researchers demonstrated that dimeric and polymeric HG129 and HG130 IgA were able to induce monocyte-mediated phagocytosis. However, difference in antigen recognition were observed, where HG129 and HG130 mediated phagocytosis HIV-1 virions and gp140 Env-coated beads, respectively.
In summary, this study showed that HIV-specific IgA MAb, induced in the Rv144 trial have the potential to mediate anti-viral responses.
Journal Article: Wills et al., 2018. HIV-1-Specific IgA Monoclonal Antibodies from an HIV-1 Vaccinee Mediate Galactosylceramide Blocking and Phagocytosis. Journal of Virology.
Article by Cheleka AM Mpande