According to a recent study, a man who received a stem cell transplant to address his cancer also showed signs of being HIV-free after the operation (Figure 1).
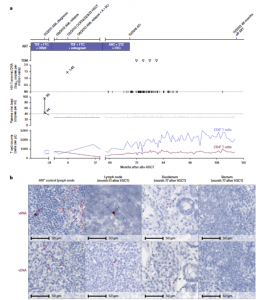
Figure 1: Clinical course and HIV-1 reservoir before and after ATI. a, Clinical
events, ART regimen, HIV-1 plasma viral load, proviral load from PBMC and CD4+ and CD8+ counts. The triangles indicate negative results in the therapeutic drug monitoring (TDM) 3, 6, 9 and 12 months after ATI. ABC, abacavir; ND, not detectable. b, In situ hybridization assays for viral DNA (vDNA) and viral RNA (vRNA) revealed HIV-1 DNA and RNA traces in lymph node tissue (month 51) and duodenum but not rectum biopsies (month 77). Left panels: untreated HIV+ control patient.
The patient, a 50-year-old male with HIV, had leukaemia and endured a stem cell transplant. He received a new immune system because of the operation, and crucially, it came from a donor with an uncommon gene mutation that makes body cells impervious to HIV infection. That happened ten years ago. According to doctors, the patient has been off HIV medications for four years and is showing no symptoms of the infection still being present in his body.
Since the patient stopped taking all anti-viral medications four years ago, they have not discovered any signs of HIV in his body. The individual is referred to as the “Dusseldorf patient” and is the third instance of his kind to be documented in the medical journals. Nearly 15 years ago, the first was detailed.
The researchers were lucky to lucky to find the stems cells, the scientists were found to find the stems cells were able to find compatible donors donors. The medical researchers were found to find the stems cells were able to find compatible donorss. The lucky lucky stem cells were carried two two stem stem stems cells carried two two two two stem stem stem stem. CCR5 gene CCR5 gene gene deletion deletes the receptors that most most HIV strains use the most
However, stem cell transplantation can be a dangerous treatment and has not been proposed as a treatment for HIV despite the results. It should only be carried out when a patient has advanced leukaemia because it is a dangerous operation with potentially fatal consequences.
The results from this and the other few instances of HIV cure, the researchers are optimistic that they will help future study to create less risky and more broadly applicable strategies for HIV curing. Studies are looking into the possibility of “editing” the CCR5 gene as a potential HIV treatment, but there are “a number of hurdles” involved.
Journal article: Björn-Erik Ole Jensen, B.E., et al., 2023. In-depth virological and immunological characterization of HIV-1 cure after CCR5Δ32/Δ32 allogeneic hematopoietic stem cell transplantation. Nature Medicine.
Summary by Stefan Botha










