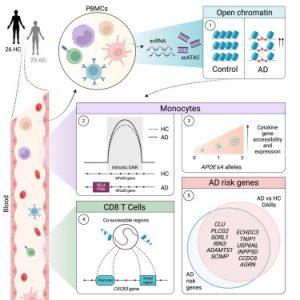
A recent study has described a fascinating connection between Alzheimer’s disease and the immune system (Figure 1). Researchers discovered that the blood of Alzheimer’s patients carries epigenetic changes, meaning their environment or behaviours have altered how their genes function.
Interestingly, many of these altered genes are linked to an increased risk of Alzheimer’s itself. This suggests a potential two-way street: genes influencing susceptibility and the disease itself triggering further changes in the immune system.
While traditional research focused on the brain’s immune system, this study delves into the peripheral immune system in the blood. The findings suggest it might play a crucial role in Alzheimer’s development.
The study revealed “open chromatin” in the patients’ immunes cells, indicating exposed genes susceptible to alteration. Additionally, a receptor called CXCR3 was found more accessible on T cells, suggesting they might be homing in on damage signals from the brain.
The jury is still out on whether these T cells are harming or helping. They could be either exacerbating the damage or attempting repairs, highlighting the complexity of immune system involvement.
Further complicating the picture, epigenetic changes were also found in inflammatory proteins within monocytes, another type of white blood cell. This adds another layer to the complex interplay between immunity and Alzheimer’s.
These findings offer intriguing insights but leave many questions unanswered. Further research is crucial to understand the exact role of the peripheral immune system, the nature of T cell activity, and whether targeting these changes could hold therapeutic potential in the fight against Alzheimer’s.
Journal article: Ramakrishnan, A., et al., 2024. Epigenetic dysregulation in Alzheimer’s disease peripheral immunity. Neuron.
Summary by Stefan Botha