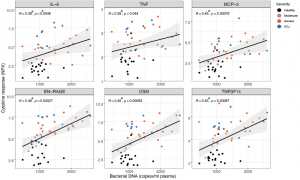
Spearman’s correlation between cytokines and bacterial DNA measured in plasma. Each dot represents a sample (n = 18 and 51 for healthy and infected, respectively). Colors of the dots indicate severity of clinical disease as shown in the legends. The boxes show median, upper and lower quartiles in the box plots. The whiskers show 5 – 95 percentiles. The differences between the groups was measured by Mann-Whitney rank sum test (*** p < 0.001).
What causes mild or severe COVID-19? A recent paper in Science used a systems biology approach to determine host immune responses to COVID-19 using an array of cellular and molecular procedures. On initial immune cell screening, the authors found an increase in plasmablasts and effector CD8 T cells in the peripheral blood and a decrease in the frequency of plasmacytoid dendritic cells. There was also a marked reduction in the ability of monocytes and myeloid DCs to produce IL-6, TNF-α and IL-1β after being stimulated with TLR ligands, indicating an impaired pro-inflammatory innate response in blood leukocytes of patients with COVID-19. Genes encoding for pro-inflammatory cytokines, as well as HLA-DR expression in myeloid cells, were also reduced. Of note, was the enhanced levels of plasma levels of EN-RAGE, TNFSF14 and OSM which correlated with the clinical severity of disease. However, in agreement with the cellular data, gene expression of both TNFSF14 and OSM were down-regulated in PBMCs from COVID-19 patients with severe disease. It is therefore likely that the plasma pro-inflammatory cytokines originate from the cells in lung tissue rather than from peripheral blood cells. The positive correlation of plasma levels of bacterial DNA and lipopolysaccharide (LPS, derived from gram negative bacteria) with the plasma levels of EN-RAGE, TNFSF14, OSM and IL-6 would support the notion that lung damage is the origin of the bacterial products that triggers a tissue-origin of hyperinflammation leading to severe COVID-19.
Journal Article: Arunachalam et al., 2020. Systems biological assessment of immunity to mild versus severe COVID-19 infection in human. Science
Summary by Clive Gray










