Lifetime daily antiretroviral treatment (ART) against HIV, is the only way to suppress HIV viral load to undetectable levels. One of the goals of the HIV treatment strategy is to develop immunotherapies that can durably induce ART-free HIV remission. Research led by Dr Anthony Fauci demonstrated the ability of an antibody, known as Vedolizumab, that targets the α4β7 in preventing HIV viral rebound in the absence of ART in non-human primates (NHPs) (Byrareddy et al., 2016; summary:HIV R4P Highlights: α4β7 antibody and ART: a novel HIV therapy.).
Why target α4β7 in the first place (you wonder) ? Many researchers, and most recently, Nawaz et al., showed that the interaction of MAdCAM with its ligand α4β7, present on the surface of CD4 T cells, costimulates T cells and thereby promotes HIV replication. Thus blocking these interactions by an anti-α4β7 antibody, could result in reduced viral replication and potentially viral suppression. (Read more: α4β7-MAdCAM interaction promotes HIV replication.)
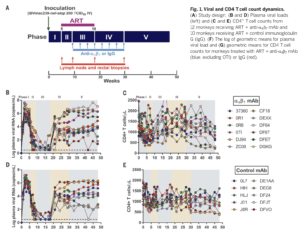
Byrareddy et al., showed that ART-treatment (short term 90 days) of Simian Immunodeficiency Virus (SIV, HIV-like virus) infected rhesus macaques followed by anti-α4β7 infusions (3-weekly), 9 weeks post infection for approximately 23 weeks could suppress viral load without the need of long term ART. This research was very promising, and initiated the testing of this strategy in a phase 1 clinical trial.
Byrareddy et al., showed that ART-treatment (short term 90 days) of Simian Immunodeficiency Virus (SIV, HIV-like virus) infected rhesus macaques followed by anti-α4β7 infusions (3-weekly), 9 weeks post-infection for approximately 23 weeks could suppress viral load without the need of long term ART. This research was very promising and initiated the testing of this strategy in phase 1 clinical trial.
Researchers have attempted to replicate Byrareddy et al., findings and 3 of these studies were recently published Science: Mascio et al., 2019; Abbink et al. 2019, Iwamoto et al., 2019. However, none of the recently published research were able to replicate Byrareddy et al., findings nor demonstrate a beneficial effect of anti-α4β7 on viral replication in the absence of ART. The discrepancies in results obtained by researchers Byrareddy et al., 2016 can not be attributed to the SIV strain used, as two of the studies used the same variant as Byrareddy et al., 2016.
Mascio et al. showed that in the absence of ART anti-α4β7 did not have any beneficial effect on preventing viral rebound nor have an effect on CD4 count in the NHP model. In fact viral replication was similar between anti-α4β7 and placebo arm, however, NHPs administered anti-α4β7 had marginally increased CD4 T cells in circulation than the placebo arm. Biopsies of the lymph node and rectal tissue also showed no difference in viral load nor proportions of infected T cells in NHPs administered with anti-α4β7 and placebo. Unfortunately, Mascio et al., could not provide a clear reason for differences in results obtained compared to Byrareddy et al., 2016. They suggested differences in results could be due to heterogeneity in NHPs and potential differences in α4β7 expression levels in the two cohorts of NHPs.
Journal Articles:
- Byrareddy et al., 2016. Sustained virologic control in SIV+ macaques after antiretroviral and α4β7 antibody therapy. Science
- Mascio et al., 2019. Evaluation of an antibody to α4β7 in the control of SIVmac239-nef-stop infection. Science
- Abbink et al. 2019. Lack of therapeutic efficacy of an antibody to α4β7 in SIVmac251-infected rhesus macaques. Science
- Iwamoto et al., 2019. Blocking α4β7 integrin binding to SIV does not improve virologic control. Science