In a recent paper by Lee, et al. investigated the neurological consequences following SARS-CoV-2 infection and subsequent COVID-19 disease. In this paper the researchers found that certain antibodies mark cells, mistakenly, lining the brain’s blood vessels for attack which leads to an inflammatory responses and tissue damage (Figure 1). This paper provides important insights into the effects of COVID-19 on the neurological status of certain individuals.
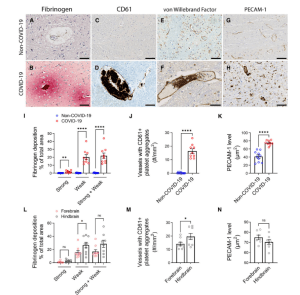
Figure 1: Microvascular injury and thrombus formation. Immunostaining for (A and B) fibrinogen, (C and D) CD61 for activated platelets, (E and F) vWF and (G and H) PECAM-1 shows absence or minimal staining in the non-COVID-19 brain but in the COVID-19 patients, there was (B) perivascular leakage of fibrinogen, (D) platelet aggregates, (F) thrombi and (H) increased PECAM-1 on endothelial cells. Significantly greater (I) leakage of fibrinogen (**P = 0.0011, ****P < 0.0001) and (J) blood vessels with platelet aggregates were present in the COVID-19 brains (****P < 0.0001). (K) PECAM-1 was significantly increased in the brains of COVID-19 patients compared to non-COVID-19 controls (****P < 0.0001). (L–N) Dots represent the average of individual values in the brain regions that make up the forebrain or hindbrain of a patient. The forebrain includes the cerebrum, basal ganglia and thalamus. The hindbrain contains the pons, medulla and cerebellum. (L) Strong fibrinogen deposition was equally distributed in different regions of the brain, while weak deposition was more prevalent in the hindbrain compared to the forebrain (*P = 0.04). (M) There were more thrombi in the hindbrain compared to the forebrain of the COVID-19 patients (*P = 0.04). (N) PECAM-1 immunostaining was equally distributed in different brain regions of the COVID-19 patients. Data represents mean ± SEM. Scale bars = 100 µm (Lee, et al., 2022).
The damage by COVID-19 on endothelial cells of blood vessels in the brain, leads to a disruption of the blood-brain barrier resulting in leakage of proteins and other particles from the blood. This may lead to clotting or bleeds which can result in a stroke. The researchers of this study were able to describe certain immune complexes that are formed on the surface of endothelial cells in the brains of patients who had unfortunately succumbed to COVID-19.
They described an antibody-mediated responses, marking endothelial cells for activation, which then express adhesion molecules which may cause clots and leakage. This process leads to recruitments of various immune cells resulting in inflammation and potential tissue damage.
This paper helps provide more information into how the immune responses causes damage in the brain after COVID-19 infection, but as to which molecule is targeted for attack still needs to be identified. Furthering our understanding of such neurological consequences from COVID-19 can help researchers develop new therapeutic tools to address long-term neurological symptoms including headache, fatigue, loss of taste and smell, sleep problems, etc.
In their own words:
“Antibody-mediated cytotoxicity directed against the endothelial cells is the most likely initiating event that leads to vascular leakage, platelet aggregation, neuroinflammation and neuronal injury. Therapeutic modalities directed against immune complexes should be considered.”
Journal article: Lee, M.H., et al., 2022. Neurovascular injury with complement activation and inflammation in COVID-19. Brain.
Summary by Stefan Botha










