New research sheds light on the complex relationship between obesity and cancer (Figure 1). We’ve known obesity is a major risk factor for cancer, but it can also strangely improve response to immunotherapy, a treatment that harnesses the immune system to fight cancer. This problem has puzzled scientists, but a team may have cracked the code, and it all hinges on surprising behaviour by immune cells called macrophages.
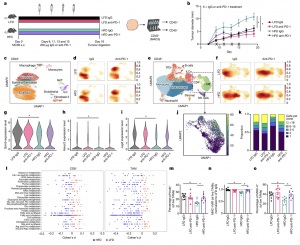
Figure 1: Obesity impairs anti-tumour immune cell function and metabolic signature. a, Schematic illustrating experimental approach. s.c., subcutaneous. b, Tumour growth of MC38 tumours over time in mice receiving IgG or anti-PD-1 treatment following 20–25 weeks of diet treatment. c, Uniform manifold approximation and projection (UMAP) embeddings of scRNA-seq profiles for CD45− cells from MC38 tumours annotated using SingleR. NKT, natural killer T cell; ILC, innate lymphoid cell. d, Density UMAPs of CD45− cells from the four treatment groups. e, UMAP of CD45+ cells from MC38 tumours annotated using SingleR. DC, dendritic cell; MDSC, myeloid-derived suppressor cell; NK, natural killer. f, Density UMAPs of CD45+ cells from the four treatment groups. g–i, Violin plot of Gzmb (g), Havcr2 (h) and Lag3 (i) gene expression within clusters identified as CD8+ T cells from scRNA-seq MC38 tumours. j, Combined UMAP of clone abundance from V(D)J sequencing of T cell clusters with productive TCRs. k, Frequency of total T cells within treatment groups with paired TCRα and TCRβ sequences from MC38 tumours. l, Compass analysis of scRNA-seq data presented as differential activity of metabolic reactions from clusters identified as CD8+ and macrophages comparing LFD IgG to HFD IgG groups partitioned by Recon2 pathways. ROS, reactive oxygen species. m, Percentage of pHrodo+ cells gated on live CD11b+F480+ TAMs from MC38 tumours. n, Mean fluorescence intensity (MFI) of MHC-I on TAMs from MC38 tumours. o, Percentage of MHC-II+ TAMs from MC38 tumours. For b, lines indicate the average tumour diameter measured over time (n = 8). For scRNA-seq (c–l), data are representative of 1 experiment, n = 3 pooled tumours from mice in each treatment group. For m–o, each data point represents a biological replicate (n = 8). Data are mean ± s.e.m. Data in m–o represent ≥2 independent experiments with ≥3 mice per treatment group pooled together. P values were calculated using a two-way analysis of variance (ANOVA) with a Fisher’s least significant difference test for multiple comparisons (b,m–o) or Wilcoxon rank-sum test (g–i). *P ≤ 0.05. The images of the needles, the tumour and the magnetic affinity cell sorting (MACS) set-up in a were created with BioRender.com.
Macrophages are like the cleaners, gobbling up debris and fighting infections. But in tumours, they can have different roles, sometimes helping and sometimes hindering. The study found that obesity ramps up the number of macrophages in tumours. More interestingly, these obese-environment macrophages cranked up production of a protein called PD-1, a target for immunotherapy drugs.
PD-1 normally acts as a brake on T cells, the immune system’s cells that kill cancer. But in obese mice, PD-1 seemed to be directly suppressing the macrophages themselves, hindering their ability to fight tumours. This explains the increased cancer risk in obesity – the immune system’s defences are dampened.
The researchers saw similar PD-1-expressing macrophages in human kidney cancer samples. Even better, biopsies from women with endometrial tumours showed that weight loss lowered PD-1 expression in these macrophages. This suggests that managing weight could improve immune response.
When they blocked PD-1 with immunotherapy drugs in the mice, the reinvigorated macrophages became potent tumour fighters, boosting T cell activity. This exciting finding suggests that therapies targeting macrophages alongside T cells could be a powerful one-two punch against cancer.
These discoveries not only explain the obesity paradox but also offer new avenues for improving immunotherapy and identifying patients most likely to benefit. With more research, macrophages could become valuable allies in the fight against cancer, especially for those battling the disease alongside obesity.
Journal article: Bader, J.E., et al., 2024. Obesity induces PD-1 on macrophages to suppress anti-tumour immunity. Nature.
Summary by Stefan Botha
