Food insecurity (FI) is a significant and growing public health concern, particularly among older adults in the United States. Approximately one in four food-insecure households includes an adult aged 65 or older, highlighting the widespread nature of this issue. Beyond its immediate impact on access to adequate nutrition, FI has far-reaching consequences, contributing to chronic diseases, mental health challenges, and heightened systemic inflammation.
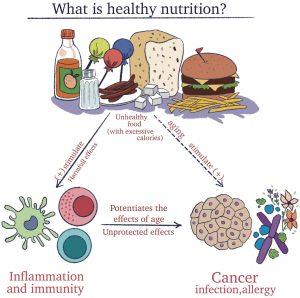
Figure 1: Chronic inflammation; Food insecurity; Health and Retirement Study; Inflammation, immune functioning; Inflammatory cytokines; Older adults.
A recent study explored the link between FI, inflammation, and immune function in older adults. Drawing on data from the Health and Retirement Study, the researchers examined how FI might exacerbate age-related declines in immune health and contribute to chronic disease susceptibility. Their findings revealed critical insights into the physiological impact of FI and underscored the need for public health interventions to support this vulnerable population.
Inflammation and Food Insecurity
Inflammation is a natural immune response, but chronic inflammation can lead to severe health problems. The study identified higher levels of inflammatory markers, including C-reactive protein (CRP) and interleukin-6 (IL-6), among food-insecure older adults. These markers are associated with systemic inflammation, which plays a pivotal role in the development and progression of chronic diseases such as cardiovascular disease, diabetes, and certain cancers. Elevated CRP and IL-6 levels are particularly concerning in older adults, as they can accelerate age-related health declines.
Chronic low-grade inflammation, often referred to as “inflammaging,” is a hallmark of aging. For food-insecure individuals, the combination of poor nutritional intake and psychosocial stress may exacerbate inflammaging. Nutritional deficiencies can weaken the body’s ability to regulate inflammation, while the stress associated with FI may further heighten inflammatory responses. Together, these factors create a vicious cycle that increases the risk of chronic illnesses and impairs overall health.
Immune Function and Cytomegalovirus
The study also investigated the relationship between FI and immune function, focusing on cytomegalovirus (CMV) seropositivity as an indicator of immune memory. CMV, a common virus that remains dormant in the body after initial infection, can reactivate in the presence of immune dysfunction. Seropositivity rates provide insights into immune health and the body’s capacity to manage latent infections.
Among food-insecure older adults, researchers found lower rates of CMV seropositivity. This suggests impaired immune function, as a healthy immune system should maintain control over latent infections like CMV. Impaired immune function increases susceptibility to infections, reduces the efficacy of vaccines, and exacerbates the challenges associated with aging immune systems. For older adults already at risk due to age-related immune decline, FI further compromises their ability to fight infections and maintain overall health.
The intersection of FI, inflammation, and immune dysfunction has broader implications for public health. Older adults facing FI are more likely to experience poor health outcomes, including increased hospitalizations, longer recovery times, and higher mortality rates. Chronic diseases driven by systemic inflammation, such as heart disease and diabetes, impose significant physical, emotional, and financial burdens on affected individuals and their families.
Mental health challenges are another critical consequence of FI. The stress and anxiety associated with not having reliable access to food can contribute to depression and other mental health disorders. These conditions can further weaken the immune system and exacerbate inflammation, creating a compounding effect that magnifies health risks.
Broader Health Implications
The findings of this study highlight the urgent need for targeted interventions to address FI among older adults. Public health strategies must prioritize improving access to nutritious food, reducing systemic inflammation, and supporting immune health. These efforts can promote healthier aging and mitigate the negative impacts of FI on older populations.
Expanding access to programs like the Supplemental Nutrition Assistance Program (SNAP) and senior-specific initiatives such as Meals on Wheels can help ensure older adults receive adequate nutrition. These programs should also emphasize the importance of nutrient-dense foods that support immune function and reduce inflammation. Local community organizations play a critical role in addressing FI. Initiatives such as food banks, community gardens, and meal delivery services can provide immediate relief while fostering social connections that enhance mental and emotional well-being.
Healthcare providers should screen for FI as part of routine care for older adults. By identifying at-risk individuals, providers can connect them with resources and services to address their needs. Integrating nutritional counseling and support into healthcare plans can also help manage inflammation and improve immune health. Addressing the systemic causes of FI requires policy-level action. Advocacy efforts should focus on expanding funding for nutrition assistance programs, increasing access to affordable healthcare, and addressing socioeconomic disparities that contribute to FI.
Food insecurity among older adults in the United States is a pressing public health issue with profound implications for inflammation, immune function, and overall health. The findings of recent research underscore the interconnectedness of FI, chronic inflammation, and immune dysfunction, highlighting the need for comprehensive interventions to support this vulnerable population. By addressing FI through nutritional programs, community support, healthcare integration, and policy advocacy, society can help ensure healthier aging and improve quality of life for older adults facing food insecurity.
Journal article: Aljahdali, A. A., Ludwig-Borycz, E., & Leung, C. W. (2024). Food insecurity, inflammation, and immune function among older US adults: Findings from the health and Retirement study. Brain, Behavior, and Immunity.
Summary by Faith Oluwamakinde










