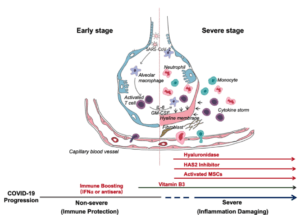
After an incubation period, the invading COVID-19 virus causes non-severe symptoms and elicits protective immune responses. The successful elimination of the infection relies on the health status and the HLA haplotype of the infected individual. In this period, strategies to boost immune response can be applied. If the general health status and the HLA haplotype of the infected individual do not eliminate the virus, the patient then enters the severe stage, when strong damaging inflammatory response occurs, especially in the lungs. At this stage, inhibition of hyaluronan synthase and elimination of hyaluronan can be prescribed. Cytokine activated mesenchymal stem cells can be used to block inflammation and promote tissue reparation. Vitamin B3 can be given to patients starting to have lung CT image abnormalities. (Source: Shi et al., 2020)
As the pathogenesis of SARS-CoV-2 infection in humans remains unclear, there is currently no specific antiviral drug against the virus. However, since most patients have mild symptoms and good prognosis after the infection, this indicates that the immune function is a strong defence against this virus.
In this sense, Lin et al., 2020 have described a hypothetical model of SARS-CoV-2 pathogenesis based on the human immune response against SARS, MERS and influenza infection. In all cases, changes in T lymphocytes subsets (lymphopenia) accompanied by the cytokine storm syndrome contribute to the progression of the disease and poor prognosis.
Regarding SARS-Cov-2, the authors suggest that the virus may enter the peripheral blood from the lungs, causing the viremia phase. The virus primarily targets cells that express ACE2, including cells from the lung, heart, renal and gastrointestinal tract. Around seven to 14 days after the onset of symptoms, the virus begins a second attack causing the patient’s condition to aggravate. During this period, lymphopenia is commonly observed, with an increase in IL-6 and other inflammatory cytokines (pneumonia phase). If the immune response is effective viral suppression occurs. However, this may not occur if the patient is 60 years of age or older and/or has other co-morbidities e.g. hypertension and diabetes.
The authors consider that the best therapeutic approaches for critical patients include intravenous immunoglobulin, anticoagulant therapy and cytokine blockade. Supporting this Shi et al., 2020, suggest using different therapeutic approaches depending on the infection phase. Specifically, the authors suggest boosting adaptive immunity potentially using anti-sera and IFN-α during the non-severe stage to control viremia, while using interventions that aim to reduce hyperinflammation and lung damage should be used during the severe (pneumonia) stage.
Journal Articles:
- Lin et al., 2020. Hypothesis for potential pathogenesis of SARS-CoV-2 infection——a review of immune changes in patients with viral pneumonia. Emerging Microbes and Infections.
- Shi et al., 2020. COVID-19 infection: the perspectives on immune responses. Cell Death and Differentiation.
Article by Christian David Barreto Vargas











