 Autoimmune hepatitis (AIH) is a chronic inflammatory liver disease that occurs at any age and mainly affects women. The pathogenesis of AIH is complex and was long unknown. Understanding the immunopathogenesis of AIH is crucial for the treatment of AIH patients and the development of novel AIH therapeutic strategies.
Autoimmune hepatitis (AIH) is a chronic inflammatory liver disease that occurs at any age and mainly affects women. The pathogenesis of AIH is complex and was long unknown. Understanding the immunopathogenesis of AIH is crucial for the treatment of AIH patients and the development of novel AIH therapeutic strategies.
Central tolerance plays an important role through the generation of tolerant T cells and elimination of autoreactive T cells. Peripheral tolerance results in the development of inducible regulatory T cells (Tregs) within the liver which is a highly tolerogenic organ. Despite these effective mechanisms, loss of tolerance in AIH can occur through a combination of genetic predisposition, environmental stimulus and an imbalance in immunological regulatory mechanisms.
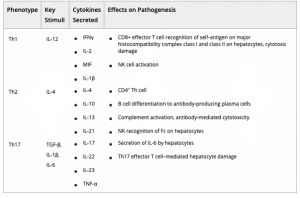
Cytokines produced locally such as IL-12 help naive T cell differentiate to a Th1, characterized by secretion of IFN-γ, IL‐2 with development of activated macrophages and effector CD8+ T cells. This will cause direct cytotoxic damage to antigen‐expressing hepatocytes. IL‐4 promotes Th2 phenotype, characterized by IL‐10, IL‐4, and IL‐13 secretion, which promotes B cell differentiation to antibody‐producing plasma cells and complement activation. Transforming growth factor β (TGF‐β) and IL‐6 result in the promotion of a Th17, principal cause of liver damage and inflammation. A dynamic balance between proinflammatory Th17 and immunosuppressive Tregs can critically determine the immunopathology of AIH. (Table 1 )
Other T cell subsets include both γδ T cells and mucosal‐associated invariant T (MAIT) cells. A recent study by Renand et al demonstrates a reduction of the peripheral Th1/ Th17 cytokine profile of memory CD4 T cells and elevation of granzyme B–producing MAIT cells in newly diagnosed patients with AIH compared with control subjects.
B cells play an important role in AIH both by generating autoantibodies and by inducing T cell responses.
But what leads to the perpetuation of T cell–mediated inflammation long after the absence of the inciting stimulus? In fact, inflammation can persist through molecular mimicry and the perpetuation of cytokine‐driven injury.
There is a lack of innovative therapies to treat AIH, therefore understanding pathogenic mechanisms is a must, especially the role of Tregs and auto-reactive B cells. Recent case reports have highlighted the potential role of B cell depletion therapy (anti‐CD20) in refractory cases of AIH. Inhibition of BAFF receptor is a novel therapeutic approach.
Journal article: Assis 2020. Immunopathogenesis of Autoimmune Hepatitis. Clinical Liver Disease
Summary by Khaoula Attia










