Researchers have now found that gingiva stiffness affects gingival fibroblast characteristics, which in turn affects whether inflammation is likely to develop and makes it challenging to create gingival fibres. (Figure 1).
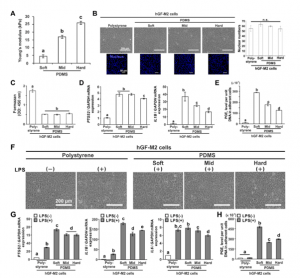
Figure 1: Effects of substrate stiffness on the proinflammatory responses of hGFs. (A) Results of Young’s modulus of PDMS substrates of soft, mid, and hard stiffness, respectively. (B,F) Representative phase microscopic images, (B) fluorescence confocal laser microscopic images of nucleus (blue) and the quantification of nuclear numbers based on images, (C) water-soluble tetrazolium (WST)-1-based colorimetry for cell attachment numbers, and (D,G) reverse transcription-polymerase chain reaction (RT-PCR)-based gene expression analysis for PTGS2, IL1B and IL6 relative to GAPDH in the hGF-M2 cells cultured on the 0.1wt% collagen-coated polystyrene culture plate and soft, mid, and hard PDMS for 12 h with or without co-incubation with 1000 ng/mL of LPS. (E,H) PGE2 levels per unit DNA in adherent hGF-M2 cells under the corresponding culture condition as above by enzyme-linked immunosorbent assay (ELISA) analysis of culture supernatants. Data are represented as the means ± standard deviation (SD; N = 4 in B, N = 3 in C-E, G and H). Different letters indicate the statistically significant difference between them (P < 0.05; Tukey’s honestly significant difference [HSD] test). hGFs human gingival fibroblasts, LPS lipopolysaccharide, PDMS polydimethylsiloxane, PGE2 prostaglandin E2, PTGS2 prostaglandin G/H synthase 2, IL1B Interleukin-1β, IL6 Interleukin-6, GAPDH glyceraldehyde-3-phosphate dehydrogenase, n.s. non-significant difference
People with dense or rigid gingiva are less likely to experience gingival recessions, as has long been known. The gingiva starts to pull back at this point, exposing the tooth’s base. In this research, human gingival fibroblasts were grown on artificial environments that replicated either soft or hard gingiva. They found that the intracellular anti-inflammatory system in the gingival fibroblasts was triggered by hard gingiva-simulated stiffness and stopped inflammation.
This study is the first to show the molecular processes at work in relation to a patient’s periodontal characteristics.
Journal article: Tiskratok, W., et al., 2023. Substrate stiffness controls proinflammatory responses in human gingival fibroblasts. Scientific Reports.
Summary by Stefan Botha










