In a recent IUIS Webinar, Eric Vivier presented data on longitudinal analysis of immune responses in the blood and bronchoalveolar lavage fluid (BALF) of patients at various stages of COVID-19 severity: paucisymptomatic, pneumonia and acute respiratory distress syndrome (ARDS). Highlights of his webinar include:
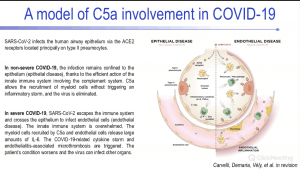
- Description of how SARS-CoV-2 (as well as SARS-CoV, MERS-CoV) N proteins bind to MASP-2, which leads to activation of complement component 5a (C5a) and aggravated lung damage. C5a has also been shown to drive pathogenesis of several viral-induced pneumonia and ARDS, and he specifically showed that levels of C5a increased with COVID-19 disease severity.
- C5a can bind to C5a receptor 1 (C5aR1) which is expressed on neutrophils and myeloid cells. He presented data that demonstrated upregulation of C5aR1+ cells in BALF from COVID-19 patients.
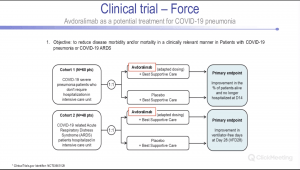
- Anti-C5aR1 therapeutic monoclonal antibodies, Avdoralimab, prevented C5a-mediated human myeloid cell recruitment and activation and inhibited acute lung injury (ALI) in human C5aR1 knockin mice. These results support C5a-C5aR1 axis blockade as a means of limiting myeloid cell infiltration in damaged organs and preventing the excessive lung inflammation and endothelialitis associated with ARDS in COVID-19 patients. (Proposed mechanism is described in the figure below)
Summary by Cheleka AM Mpande