Melanoma patients with spreading cancer face a treatment dilemma – existing therapies offer limited guidance on who will benefit and for how long. A new study sheds light on this challenge by identifying a promising liquid biopsy biomarker for personalized treatment decisions.
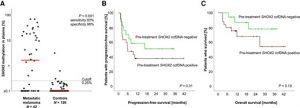
Figure 1: SHOX2 ccfDNAm and its association with survival in melanoma patients treated with palliative immunotherapy. SHOX2 ccfDNAm levels in blood plasma at baseline (pretreatment) of n = 42 patients with metastatic (stage IIIC–IV) melanoma treated with palliative anti-PD-1 immunotherapy compared to n = 126 individuals without evidence of malignant disease (A). Kaplan–Meier estimates of progression-free (B) and overall survival (C) in metastatic melanoma patients stratified according to pretreatment SHOX2 ccfDNA positivity (>0.25% cutoff). P values refer to Mann–Whitney U-test and log-rank test, respectively.
While therapies exist for advanced melanoma, a critical gap remains in predicting which treatment works best for each patient and for how long it remains effective. This often leads to a trial-and-error approach, wasting precious time and exposing patients to potentially ineffective treatments.
Researchers have discovered a potential game-changer: a specific biomarker in a liquid biopsy that can predict a patient’s response to immunotherapy at an early stage. This paves the way for more personalized treatment plans for melanoma patients.
Immunotherapy with PD-1 inhibitors is a common treatment for melanoma, but it’s not a one-size-fits-all solution. Some patients either don’t respond initially or develop resistance over time. The new study offers a potential path to address this challenge.
The study focused on analyzing blood samples from melanoma patients and healthy controls to identify biomarkers. They discovered that a specific biomarker, SHOX2 methylation in circulating cell-free DNA, originates directly from tumor cells and is present in the bloodstream.
The findings were encouraging. SHOX2 methylation levels were elevated in 60% of melanoma patients, while minimal levels were found in the control group. Significantly, patients with initially high levels that decreased after four weeks of treatment showed a particularly good response to the therapy.
These results suggest that SHOX2 methylation in blood has the potential to predict a patient’s response to anti-PD-1 therapy. A blood test for this biomarker could revolutionize melanoma treatment by enabling doctors to tailor therapy decisions based on individual patient responses, maximizing effectiveness and minimizing wasted time on ineffective treatments.
This study offers a glimpse into the future of personalized medicine for melanoma. By harnessing the power of liquid biopsies and identifying key biomarkers, researchers are paving the way for more effective and targeted treatment strategies for cancer patients.
Journal article: Simon Fietz et al, 2024. Circulating Cell-Free SHOX2 DNA Methylation Is a Predictive, Prognostic, and Monitoring Biomarker in Adjuvant and Palliative Anti-PD-1-Treated Melanoma, Clinical Chemistry.
Summary by Stefan Botha










