Cervical cancer, one of the top 5 common cancers in women globally, is often associated with high-risk human papillomavirus (HPV) infections such as oncogenic HPV16 and HPV18. HR-HPV oncoproteins -E5, E6 and E7- are the main viral factors implicated in the initiation and progression of CC. E6 and E7 disrupt p53 and Rb functions, molecules that are important for cellular transformation. Additionally, alterations of different cellular pathways induce genomic instability, high proliferation rates, immune response evasion, and others. HPV gene transcription is controlled by two promoters whose activation is regulated by the differentiation state of the infected cell and the polycistronic mRNAs are further regulated by alternative splicing. Interestingly, alternative splicing within E6-E7 open reading frames has been exclusively observed in HR-HPV, leading to different shorter E6 mRNA transcripts E6*I, E6*II, being E6*I the most abundant spliced E6. Remarkably, HPV16 appears to transcribe all isoforms, but HPV18 transcribe only the E6*I.
Furthermore, a key player during the carcinogenic process is interleukin-6 (IL-6), which is highly upregulated in many types of cancers and is considered a crucial cytokine during tumorgenesis. In CC, IL-6 induce angiogenesis and its expression is higher in CC tissue when compared to non-tumorigenic adjacent tissue. This over expression is correlated with tumor size and poor prognosis.
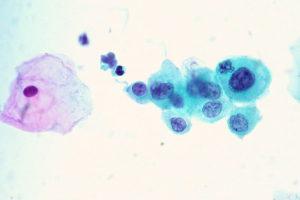
Artaza-Irigaray, et al., evaluated the influence of HR-HPV and LR-HPV oncoproteins on IL-6 expression in keratinocytes and whether this influence is mediated through p53. They report that IL-6 is highly expressed in HPV infected cervical cancer derived cell lines (HeLa and SiHa) compared to non-tumorigenic keratinocytes (HaCaT), and in cervical intraepithelial neoplasia grade 1 (positive to HPV16 and HPV18 infection) compared to HPV negative samples without lesions.
Moreover, using lentiviral vectors, they generated HaCaT cells that express E5, E6 and E7 proteins from HR-HPV (16 and 18) and low risk-HPV (62 and 84) to analyse their regulation over IL-6. They found that E5 proteins do not modify IL-6 expression, while E7 modestly increase it. E6 proteins in HaCaT highly upregulated IL-6 expression (mRNA and protein). Interestingly, the HaCaT cells that only expressed truncated E6* from HPV16 and HPV18 and a higher expression of IL-6 was observed. In contrast, the HaCaT cells that express E6 from HPV62 and HPV84 have the full length E6 protein and IL-6 expression was upregulated but not so drastically as HR-HPV. It’s worth noting that HaCaT cells have a mutated p53 form that is not degraded by E6/E7, so it seems that the regulation of IL-6 is independent of p53. These results confirm that HPV oncoproteins are able to regulate pro-inflammatory cytokines like IL-6 in order to maintain a highly proliferative microenvironment that lead to cervical tumorigenesis.
Journal Article: Artaza-Irigaray et al., 2019. E6/E7 and E6∗ From HPV16 and HPV18 Upregulate IL-6 Expression Independently of p53 in Keratinocytes. Frontiers in Immunology
Article by Christian David Barreto Vargas