Stroke and other cerebrovascular diseases inflict substantial damage to brain cells by disrupting blood flow, leading to profound neuronal impairment. Current recovery prospects for patients are often limited, with many experiencing severe physical disabilities and cognitive challenges.
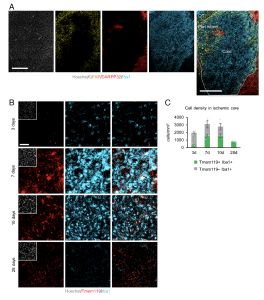
Figure 1: Microglia/macrophages accumulate in the ischemic core after tMCAO. (A) Representative images of staining for GFAP (yellow), DARPP32 (red), and Iba1 (cyan) in the ischemic striatum at 7 d after tMCAO. White dashed enclosure shows the peri- infarct area. Nuclei were stained with Hoechst (Scale bars, 500 μm). CC, corpus callosum. (B) Spatiotemporal distribution of microglia/macrophages after tMCAO. Representative images of staining for Tmem119 (red) and Iba1 (cyan) in the ischemic core of the striatum at 3, 7, 10, and 28 d after tMCAO. Nuclei were stained with Hoechst (Scale bar, 50 μm). (C) Quantification of indicated marker- positive cells in the ischemic core in (B) (n = 4 per group).
A new study has uncovered a promising avenue for treating stroke-induced brain injury by harnessing the power of immune cells to regenerate neurons (Figure 1). This finding suggests that converting immune cells into neurons might offer a compelling strategy for restoring brain function after a stroke, potentially transforming stroke care for humans.
The study concentrated on microglia, primary immune cells in the central nervous system tasked with clearing damaged brain cells. Researchers explored the potential of these cells to transform into neurons as a response to stroke-related injuries. In a mouse model mimicking stroke, researchers observed motor function impairment and significant neuron loss in the striatum, a critical brain region governing decision-making and motor coordination.
Scientists employed a lentivirus to introduce NeuroD1 DNA into microglial cells at the injury site. NeuroD1, a protein promoting neuronal conversion, facilitated the gradual transformation of infected cells into neurons. Over ensuing weeks, these newly formed neurons integrated into the brain’s circuits.
Within three weeks post-infection, mice displayed remarkable improvement in motor function, evident through behavioral assessments. Notably, removal of the newly induced neurons resulted in the reversal of these improvements, emphasizing the direct role of these converted neurons in fostering recovery.
These findings provide a new perspective on stroke treatment. Reprogramming immune cells into functional neurons presents a potential therapeutic avenue for stroke-induced brain injuries, offering hope for enhanced recovery and improved outcomes in human patients. This study marks a significant leap forward in stroke care, potentially revolutionizing how we approach neurological rehabilitation after strokes.
Journal article: Irie, T., et al., 2023. Direct neuronal conversion of microglia/macrophages reinstates neurological function after stroke. Proceedings of the National Academy of Sciences.
Summary by Stefan Botha










