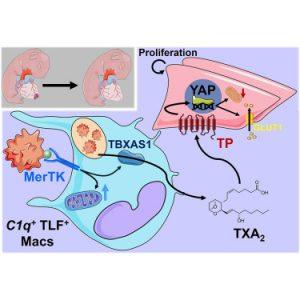
In newborns, macrophages facilitate heart regeneration through a process called efferocytosis, where they engulf and remove dying cells. This process triggers the release of thromboxane A2, a bioactive lipid that signals nearby heart muscle cells to divide and repair damage.
However, in adults, macrophages produce much lower levels of thromboxane A2, resulting in inefficient repair and the formation of scar tissue, which can lead to heart failure.
A new study has uncovered a key difference in how immune cells contribute to heart tissue regeneration in newborns versus adults after a heart attack (Figure 1). The research reveals how macrophages, a crucial component of the immune system, play a central role in stimulating heart muscle repair in newborns but fail to do so in adults. These findings could pave the way for regenerative treatments aimed at restoring heart function following injury.
To investigate these differences, researchers compared the immune response to heart injury in newborn mice (one day old) and adult mice (eight weeks old). Their analysis showed that:
- Newborn macrophages express higher levels of MerTK, a receptor responsible for detecting and engulfing dying cells.
- Blocking MerTK in newborn mice eliminated their ability to regenerate heart tissue, making their healing process resemble that of adults.
- Macrophages in newborns release thromboxane A2, which triggers heart muscle cells to multiply and repair damage.
- Heart muscle cells in newborns are metabolically primed to respond to thromboxane A2, allowing them to adapt and support regeneration.
In contrast, adult macrophages do not produce enough thromboxane A2, limiting their ability to promote tissue regeneration and instead leading to permanent scarring.
These findings suggest that mimicking the effects of thromboxane A2 in adults could enhance heart repair following injury. By harnessing the regenerative properties of newborn immune cells, researchers hope to develop novel therapies that could reprogram macrophages to promote cardiac healing in adult patients.
These findings offer new hope for cardiac regeneration, bringing science one step closer to developing innovative therapies for heart disease patients.
Journal article: Connor Lantz, C., et al., 2025. Early-age efferocytosis directs macrophage arachidonic acid metabolism for tissue regeneration. Immunity.
Summary by Stefan Botha