In a recently published paper, researchers investigated the mechanisms that underlie the timing of labour in humans, particularly spontaneous preterm labour, which is associated with increased perinatal mortality and morbidity. The study characterizes the cells at the maternal-fetal interface (MFI) in term and preterm pregnancies in both the labouring and non-labouring state in black women, who have among the highest preterm birth rates in the U.S. Using mass cytometry to obtain high-dimensional single-cell resolution, the study identified 31 cell populations at the MFI, including 25 immune cell types and six non-immune cell types. The study suggests that the PD1/PD-L1 pathway at the MFI may perturb the delicate balance between immune tolerance and rejection and contribute to the onset of spontaneous preterm labour. The study identified that PD-L1+ maternal (stromal) and fetal (extravillous trophoblast) cells were less abundant in preterm labouring compared to term labouring women. The expression of CD274, the gene encoding PD-L1, was significantly depressed and less responsive to fetal signaling molecules in cultured mesenchymal stromal cells from the decidua of preterm compared to term women.
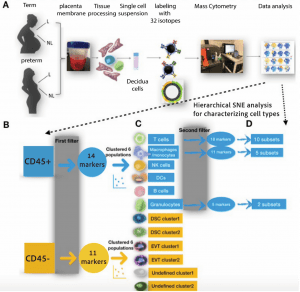
Figure 1: Experimental design and workflow. (A) Preparing decidual tissues for single cell analysis on the CyTOF platform. Our study included tissues from 16 term labouring, 12 term non-labouring, 11 preterm labouring, and 14 preterm non-labouring pregnancies (see Table 1). See Supplementary Methods for antibody staining with 32-antibody panel and CyTOF analyses. (B) After data processing and QC, the cells were first divided into CD45+ (immune) and CD45- (non-immune) pools, then characterized using two additional filters for hierarchical SNE analysis. (C) The first filter identified six immune cell types and six non-immune cell populations by 14 and 11 markers, respectively. (D) The second filter identified 10 T cell subsets, five macrophage/monocyte subsets, and two granulocyte subsets. L labouring, NL non-labouring. DCs Dendritic cells, DSC Decidual stromal cell, EVT extravillous trophoblast. Undefined: No cell-surface markers to identify the cell type.
Results:
The study found that PD-L1+ maternal (stromal) and fetal (extravillous trophoblast) cells were less abundant in preterm labouring compared to term labouring women. The expression of CD274, the gene encoding PD-L1, was significantly depressed and less responsive to fetal signalling molecules in cultured mesenchymal stromal cells from the decidua of preterm compared to term women. These results suggest that the PD1/PD-L1 pathway at the MFI may contribute to the onset of spontaneous preterm labour.
Limitations:
The paper has some limitations. The study only included one demographic, so the results may not be generalizable to other populations. Additionally, the study did not investigate the functional consequences of the observed changes in PD-L1 expression. Finally, the study did not investigate the role of other immune checkpoint molecules in the onset of spontaneous preterm labor.
The paper suggests that without more data points, including some before 20 weeks, it is not possible to further interpret the data. The study’s results should be considered suggestive, requiring replication or functional validation in independent studies. Despite these limitations, the study revealed novel findings that further our understanding of spontaneous preterm labor.
Journal article: Aneas, L.X., et al. 2023. Single cell profiling at the maternal–fetal interface reveals a deficiency of PD-L1+ non-immune cells in human spontaneous preterm labor. Scientific Reports.
Summary by Gaurang Telang










