Hidradenitis suppurativa (HS) is a chronic and debilitating inflammatory skin condition that causes painful bumps or boils beneath the skin’s surface, often in areas prone to sweating and friction, such as the armpits, groin, buttocks, and breasts. These lesions can rupture, leading to significant discomfort and scarring. Hidradenitis suppurativa affects approximately 1% to 2% of the population, particularly within the 16–40 age group, with women of African American descent being disproportionately impacted. Despite available treatments that aim to reduce symptoms, there is no cure, and the disease continues to impact the quality of life of those affected, both physically and socially.
In a recent study, researchers made a potential breakthrough in the treatment of HS. The research identified a critical interaction between two proteins—CD2 and CD58—that drives the inflammatory processes associated with HS (Figure 1). By disrupting this interaction, the researchers demonstrated the ability to suppress gene expressions linked to HS symptoms, offering a potential new therapeutic approach.
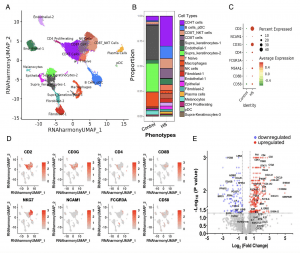
Figure 1: Innate and adaptive immune and nonimmune cells in HS lesion. (A) UMAP of cell populations from normal (NS; n = 4) and HS (n = 6) skin. The scRNAseq dataset from 27,442 cells were clustered using Seurat 4.0 and annotated to 19 clusters of immune and nonimmune cell populations. (B) Proportion of annotated cell population in each cluster from NS and HS. (C) Dot plot depicting normalized expression of genes defining selected cell lineage/function in NS and HS defining genes. (D) Feature plot showing cluster localization of selected cell lineage/function-defining genes. (E) Volcano plot of differentially expressed genes in HS (n = 8) relative to NS (n = 6 to 8) determined using qPCR arrays.
The study found that CD2, a lymphocyte cell surface protein, is expressed at elevated levels on immune cells in HS lesions, particularly on T lymphocytes and innate lymphocytes such as natural killer (NK) cells, natural killer T (NKT) cells, and mucosal-associated invariant T (MAIT) cells. These immune cells were identified as predominant players in HS lesions, perpetuating inflammation through the interaction of CD2 with CD58, another surface protein. This interaction activates T cells and innate lymphocytes, leading to the release of inflammatory molecules, including cytokines, chemokines, and growth factors, which contribute to the disease’s progression.
By blocking the CD2:CD58 interaction, the research team was able to mitigate the gene expression and secretion of these inflammatory proteins, highlighting the potential for targeting this pathway as a novel therapeutic strategy.
The research team emphasized the importance of mapping the immune cell and epithelial interactions in HS at various stages of the disease. By doing so, they hope to develop targeted interventions that address the root causes of the condition. The disruption of the CD2:CD58 interaction represents a promising therapeutic avenue, with the potential to transform the treatment landscape for HS and improve the lives of those affected by this painful and often stigmatizing disease.
Journal article: Mahendra Pratap Kashyap et al, 2024. CD2 expressing innate lymphoid and T cells are critical effectors of immunopathogenesis in hidradenitis suppurativa, Proceedings of the National Academy of Sciences.
Summary by Stefan Botha










