Allergic reactions, characterized by symptoms like itching and sneezing, can significantly impact quality of life. While some individuals are particularly sensitive to allergens like dust or pollen, others seem largely unaffected. A recent study has shed light on why this disparity exists, uncovering a specific pathway through which immune and nerve cells interact to trigger allergic responses (Figure 1).
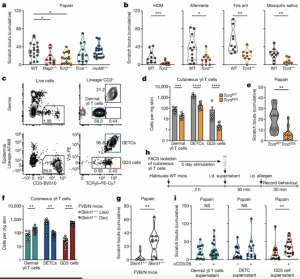
Figure 1: γδ T cells promote allergic itch through a secreted factor. a, Cumulative cheek scratch bouts following i.d. injection with papain (n = 19 WT (C57BL/6); n = 11 Rag2−/−; n = 16 Tcrd−/−; n = 13 Tcra−/−; n = 18 muMT−/−). b, Cumulative cheek scratch bouts following i.d. injection with HDM (n = 10 WT; n = 12 Tcrd−/−), Alternaria (n = 12 WT; n = 11 Tcrd−/−), fire ant (n = 9 per group) or mosquito saliva (n = 10 WT; n = 8 Tcrd−/−). c, Flow cytometry of dermis or epidermis, from naive WT pinnae. d,f, Flow cytometric quantification of skin (dermis + epidermis) γδ T cells from pinnae (d, n = 9 TcrdWT; n = 10 TcrdGDL; f, n = 8 Skint1+/+; n = 10 Skint1−/−) of TcrdGDL mice (d) or Skint1−/− mice (f). e,g, Cumulative cheek scratch bouts following i.d. injection with papain (e, n = 9 TcrdWT; n = 10 TcrdGDL; g, n = 9 Skint1+/+; n = 10 Skint1−/−) of TcrdGDL mice (e) or Skint1−/− mice (g). h, Schematic of γδ T cell supernatant transfer and behaviour protocol. i, Cumulative cheek scratch bouts following i.d. injection of γδ T supernatant, then papain (n = 16 dermal γδ T cell unstimulated; n = 20 dermal γδ T cell αCD3/28; n = 13 DETC unstimulated, DETC αCD3/28 or GD3 unstimulated; n = 15 GD3 αCD3/28). Symbols represent individual mice. Violin plots show the median and quartiles. Bar plots are mean ± s.e.m. Data represent at least two independent experiments and were combined. Statistical tests: ordinary one-way ANOVA with Tukey’s multiple comparisons test (a), two-sided unpaired t-test (b, Alternaria, fire ant, mosquito saliva) or two-sided Mann–Whitney U-test (b, HDM; d–g,i). *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001; NS, not significant. Schematics in h created using BioRender (https://biorender.com).
Researchers have identified a key role played by a particular type of immune cell, known as GD3 cells. These cells produce a molecule called IL-3, which primes sensory neurons in the skin to become more reactive to allergens. This heightened sensitivity can lead to itching and other allergic symptoms.
The study found that by targeting IL-3 or GD3 cells, it may be possible to prevent or reduce allergic responses. This discovery opens up new avenues for developing potential treatments for allergies.
Previous research had suggested that the sensory nervous system plays a crucial role in detecting allergens. However, the specific mechanisms involved remained unclear. The new findings provide a more detailed understanding of how immune and nerve cells interact to produce allergic reactions.
By uncovering this pathway, scientists may be able to develop targeted therapies that can prevent or treat allergies more effectively. Additionally, understanding the factors that activate GD3 cells could potentially lead to strategies for preventing allergic sensitization altogether.
While further research is needed to fully explore the implications of these findings, the study represents a significant step forward in our understanding of allergies. By targeting the IL-3-mediated signaling pathway, scientists may be able to develop novel treatments that offer relief to millions of people affected by allergic conditions.
Journal article: Flayer, C.H., 2024. A γδ T cell–IL-3 axis controls allergic responses through sensory neurons. Nature.
Summary by Stefan Botha










