The resident immune cells in the brain called microglia, which can damage brain tissue if triggered incorrectly, are the target of many of the immunity-focused Alzheimer’s medicines currently being developed. According to a new study, microglia collaborate with T cells, another form of immune cell, to induce neurodegeneration. (Figure 1).
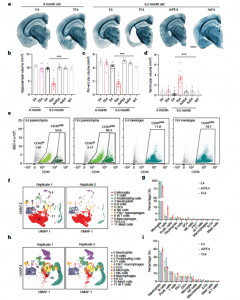
Figure 1: Immune scRNA-seq reveals increased proportion of T cells in the context of tau-mediated neurodegeneration. a, Representative images of 6-month-old E4 and TE4, and 9.5-month-old E4, TE4, A/PE4 and 5xE4 mouse brain sections stained with Sudan black. Scale bar, 1 mm. b–d, Volumes of hippocampus (b), piriform–entorhinal cortex (piri–ent ctx) (c) and posterior lateral ventricle (d) in 6-month-old E4 and TE4, and 9.5-month-old E4, TE4, A/PE4, 5xE4 and WT mice (6-month E4: n = 3; 6-month TE4: n = 7; 9.5-month E4: n = 15; 9.5-month TE4: n = 13; 9.5-month A/PE4: n = 7; 9.5-month 5xE4: n = 6; 9.5-month WT: n = 6). Data are mean ± s.e.m.; *** P < 0.0001 for 9.5-month TE4 versus A/PE4; TE4 versus 5xE4; TE4 versus E4; and TE4 versus WT (one-way analysis of variance (ANOVA) with Tukey’s post hoc test). e, Fluorescence- activated cell sorting of CD45 total and/or CD45 hi cells from brain parenchyma and meninges from E4, A/PE4 and TE4 mice for immune scRNA-seq. f, CD45 total immune cells from brain parenchyma assigned into 12 cell types as visualized by uniform manifold approximation and projection (UMAP) plots. DCs, dendritic cells; ILCs, innate lymphocyte cells. g, Bar plot showing the proportions of the 12 cell types of immune cells in the brain parenchyma. Data are mean ± s.e.m.; two biologically independent samples were used, and samples were sequenced in n = 2 batches from the E4 and TE4 groups. Prolif., proliferating. h, CD45 total immune cells from meninges assigned into 12 cell types as visualized by UMAP plots. i, Bar plot showing the proportions of the 12 cell types of immune cell in the meninges. Data are mean ± s.e.m.; two biologically independent samples were used, and samples were sequenced in n = 2 batches from the E4 and TE4 groups.
Researchers found that microglia draw potent cell-killing T cells into the brain of rodents with brain damage similar to Alzheimer’s caused by the protein tau, and that most neurodegeneration could be prevented by preventing the T cells’ entrance or activation. The authors of this research proposed that targeting T cells is an alternative strategy for halting neurodegeneration and treating tauopathies, a group of tau-related illnesses that include Alzheimer’s disease.
There are two major stages to Alzheimer’s development. Amyloid beta protein clumps first start to develop. The plaques may accumulate for many years without having any apparent impacts on mental health. However, ultimately tau also starts to consolidate, indicating that the second phase has begun. The illness then rapidly gets worse from there.
They looked for changes in the immune cell population that take place over the course of the illness in the brains of mice whose immune systems had been genetically altered to imitate various aspects of Alzheimer’s disease in humans. The brains of tau rodents contained significantly more T cells than the brains of amyloid or control mice, according to the experts. In the brains of individuals who had perished from Alzheimer’s disease, T cells were equally prevalent at locations of tau aggregation and neurodegeneration.
Researchers have worked very hard to develop treatments that stop neurotoxicity by influencing tau or microglia. They haven’t, however, examined how we can alter T cells to stop dementia.
Journal article: Chen, X., et al., 2023. Microglia-mediated T cell infiltration drives neurodegeneration in tauopathy. Nature.
Summary by Stefan Botha










