COVID-19 has presented unprecedented challenges to global healthcare, revealing the complexity of its systemic and pulmonary immunopathology. Understanding the diverse immune responses to SARS-CoV-2 is crucial in identifying biomarkers that can predict patient outcomes. This blog post summarizes a comprehensive study on integrating systemic and pulmonary immunopathology to identify these critical biomarkers.
The aim of the study is to elucidate the complex immune responses involved in COVID-19 to identify biomarkers that predict different clinical outcomes. The research focuses on both systemic and pulmonary immunopathology to understand how they contribute to disease progression. By integrating data from various immune responses, the study seeks to develop predictive models for patient outcomes. The ultimate objective is to improve clinical decision-making and personalize treatment strategies for COVID-19 patients.
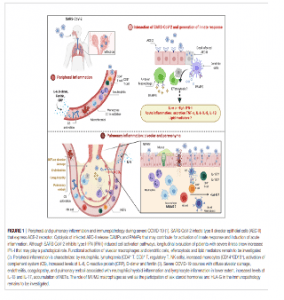
The study investigates the systemic immune response, focusing on cytokine storms and hyperinflammation, which are critical in severe COVID-19 cases. It highlights the role of various cytokines, such as IL-6 and TNF-α, in driving systemic inflammation and their potential as biomarkers for disease severity.
The pulmonary aspect examines the local immune response within the lungs, including alveolar damage, immune cell infiltration, and the development of acute respiratory distress syndrome (ARDS). The research identifies key factors contributing to lung injury and recovery, providing insights into targeted treatments for respiratory complications.
By integrating data from systemic and pulmonary studies, the researchers identify specific biomarkers that correlate with different disease outcomes. These biomarkers can help in predicting patient trajectories, from mild illness to severe disease requiring intensive care.
The study discusses the potential for using identified biomarkers to guide therapeutic interventions. Personalized treatment strategies based on biomarker profiles could enhance the effectiveness of therapies and improve patient outcomes.
The study identifies several biomarkers linked to severe COVID-19 outcomes, including elevated levels of cytokines like IL-6 and IL-8, which are associated with hyperinflammatory responses. Additionally, the presence of specific immune cell populations, such as exhausted T cells, was found to correlate with worse clinical outcomes. These findings highlight the importance of both systemic inflammation and localized pulmonary immune responses in determining the severity of COVID-19.
Identifying these biomarkers has significant implications for managing COVID-19. It enables the development of targeted therapies aimed at modulating the immune response, potentially reducing the severity of the disease. Furthermore, these biomarkers can aid in stratifying patients based on their risk, allowing for more personalized and effective treatment plans. Future research will focus on validating these biomarkers in larger cohorts and exploring their utility in other infectious diseases.
The integration of systemic and pulmonary immunopathology provides a comprehensive understanding of the immune responses in COVID-19. By identifying biomarkers associated with different outcomes, this study paves the way for improved treatment strategies and better patient management. The ongoing research in this area holds promise for enhancing our response to COVID-19 and other similar infectious diseases.
Journal articles:
- et al., 2024. COVID-19: Integrating the Complexity of Systemic and Pulmonary Immunopathology to Identify Biomarkers for Different Outcomes. Journal of Immunology Research.
- et al., 2023. The Role of Cytokines in COVID-19 Severity. Medical Science Review.
Summary by Faith Oluwamakinde