- Patient presentation
- History
- Differential Diagnosis
- Examination
- Investigations
- Discussion
- Treatment
- Final outcome
- References
- Evaluation - Questions & answers
- MCQ
Patient presentation
A three month old male infant presents to the emergency department with a one day history of haematochezia and haematuria, accompanied by a diffuse rash and shortness of breath.
Acknowledgement
This case study was kindly provided by Dr Bhadrish J Mistry, Paediatrician, Department of Paediatrics, Chris Hani Baragwanath Hospital and the University of Witwatersrand.
Partnership
We have partnered with The International Union of Basic and Clinical Pharmacology (IUPHAR) to bring you in-depth information about drugs and pharmacology with links to the Guide to ImmunoPharmacology.
History
A three month old male infant was brought into the emergency department by his mother with a first time presentation of haematochezia and haematuria, noted in his nappy. She also complained that he was short of breath and she had noted a rash that had appeared on his face, body and legs that morning.
There was no accompanying haematemesis, diarrhoea, vomiting or fever.
She also noted that he was not feeding as well as usual.
Past Medical History
The infant had been admitted to hospital in Zimbabwe at 2 months of age for “breathing problems” but no diagnosis had been given. During his admission he was transfused with packed red cells for anaemia and was discharged on iron and bactrim.
Birth History
Mother was 41 years old, P3G4
At 24 weeks gestational age, the mother was treated with 3 days of chloroquine for a possible case of malaria. The symptoms resolved and she went on to have an uneventful remainder of her pregnancy. The infant was born term, NVD with no complications during the delivery.
The infant was both breast and formula fed, duration was not specified.
Social History
The family are from Zimbabwe, now living in Johannesburg for the last month. The infant was born in Zimbabwe and lived there for the first two months of his life.
He has three older siblings aged 3, 6 and 8 who are all well
Vaccinations
Up to date
Medication
Currently completing a course of iron and bactrim. No history of any traditional medication use (orally or via enema).
Allergies
None known
Differential Diagnosis
- Post streptococcal glomerulonephritis
- Perforated meckel’s diverticulum
- Salmonella
- Shigella
- ITP
- DIC
- Neonatal Lupus Erythematosus (NLE)
Examination
Vitals
Heart Rate- 120 beats per minute Blood Pressure- 80/50 Respiratory rate- 40 breaths per minute Temperature- 36.5°C
Anthropometry
Weight: 4.4kg (75% expected weight for age)
Length & head circumference: Normal
General
Marked pallor
No jaundice
No significant lymphadenopathy
No oedema
Subtle dysmorphic features:
- Biparietal prominence
- Epicanthic folds
- Almond shaped eyes
Subconjunctival haemorrhage right eye
No cataracts
No subaponeurotic haemorrhage or cephalhaematoma
Skin
Diffuse petechiae and purpura involving face, trunk and limbs
No ecchymosis
Abdomen
Mildly distended but soft & non tender
Hepatomegaly: 4-5cm firm, non tender
Splenomegaly: 2-3cm & firm
Bowel sounds present
Chest
Moderate respiratory distress
Clear on auscultation
Cardiovascular
Tachycardia & hypotensive
No evidence of congestive cardiac failure
Neurological
No focal neurological signs
Musculoskeletal
No abnormalities
Investigations
| Values | Normal Limits | |
|---|---|---|
| WBC | 3.1 (diff 1.6 neutrophils and 2.8) | (4-12x109/l) |
| HB | 4.0999999999999996 | (12.1-15.2g/l) |
| MCV | 78.8 | (80-96 fl) |
| Platelets | 15 | (140-45x109/l) |
| Reticulocyte count | 5.6000000000000001E-2 | (0.8-4% RBC) |
| Smear: | ||
| Normochormic, normocytic anaemia with spherocytes | ||
| Red cell fragments | ||
| Left shift in neutrophils | ||
| LDH | 953 | (70-250 u/l) |
| Haptoglobin (free serum) | 0.45 | (27-139 mg/dl) |
| Coombs direct | Positive | |
| INR | 0.9 | (1.0-1.3) |
| PTT | 30 | (23-31) |
| WR | Negative | |
| TPHA | Negative | |
| Toxoplasmosis | Negative | |
| Rubella | Negative | |
| Parvovirus B19 | Negative | |
| Malaria | Negative | |
| Herpes | Negative | |
| CMV | Negative | |
| Total bilirubin: | 22 | (3-17 umol/l) |
| Uncongugated bilirubin: | 15 | (0.0-0.3 mg/dl) |
| ANA | Positive | |
| Anti Ro: | 104 | |
| Anti La: | 156 | |
| ACLA: IgG | 18 | |
| ACLA IgM | 12 | |
| B2 glycoprotein | Normal |
Mothers Results
WR: negative
ANA: Positive, titre 1280 speckled pattern
dsDNA: negative
Anti Ro: 96
Anti La: 144
Abdominal ultrasound
Features of hepatomegaly
Splenomegaly with multiple microabscesses
Very thickened bladder with dilated post urethra
Bone marrow trephine
Reactive changes in RBC and megakaryopoeitic precursor
Focus granulation tissue secondary to previous haemorrhage
No granulomatous infiltration
No neoplastic infiltrate
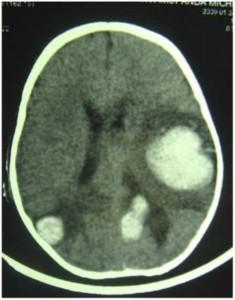
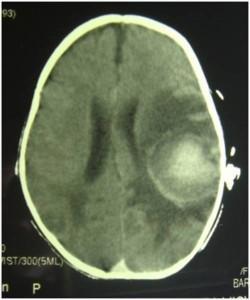 CT Brain
CT Brain
Day 16 post admission, infant developed a seizure.
CT scan shows multiple parenchymal bleeds and oedema
29 Days later CT scan shows decreased bleeding and oedema.
Discussion
Neonatal lupus erythematosus (NLE) is an uncommon condition associated with maternal anti-Ro and anti-La autoantibodies. These autoantibodies are passively transferred to the foetus through the placenta, and once in the foetal circulation promote the development of NLE by binding to antigen. Anti-Ro and anti-La autoantibodies bind to nuclear antigens translocated to the cell membranes of apoptotic cells, in particular myocardiocytes and keratinocytes. Macrophages expressing Fc receptors recognise bound IgG and become activated and initiate inflammatory responses. This antigen binding is found to cause cutaneous lupus lesions, third-degree heart block, cardiomyopathy, hepatobiliary disease, and thrombocytopenia or other haematologic cytopenias. In this case study we see cutaneous and hepatic involvement accompanied by a pancytopaenia. Studies have found that anti La antibodies are associated with cutaneous lupus and anti Ro antibodies are associated with congenital heart block. Anti-platelet antibodies are present which cause destruction of platelets while anaemia is caused by both antibodies and haemorrhage. In this case haemorrhage is evidenced by haematochezia, haematuria and intracranial bleeds. Pancytopaenia is also further exacerbated by hypersplenism which can result in patients undergoing splenectomy if the condition is not resolved. Typically only one organ is affected in NLE, but any combination of organ involvement may occur. Pregnant women with anti-Ro and anti-La antibodies have a 5-20% risk of having a child/children with NLE, with the risk being highest in mother’s with high titre antibodies.
Although during pregnancy, maternal IgG autoantibodies are transported to the foetus via the placenta after birth the foetal levels of Ro and La IgG autoantibodies are found to rapidly decrease suggesting that after placental detachment the source of immunoglobulins is markedly decreased or ended. Although breast milk also contains IgA and IgG autoantibodies the dose or foetal uptake is not enough to reach detectable levels.
The most common severe manifestation of neonatal lupus is third-degree heart block, which usually begins during the second trimester of gestation and once established is irreversible. This is thought to occur from the inflammatory process that results from the macrophages expressing Fc receptors which recognise the bound IgG. The secretion of pro-inflammatory cytokines causes inflammation and ultimately fibrosis in the cardiac tissue. These patients require the insertion of a pacemaker to maximize heart function. If cardiomyopathy is also present this can be fatal.
Otherwise for the most part NLE is transient. The cutaneous lesions are what give the neonatal “lupus” its name, as the lesions are clinically and histologically consistent with cutaneous lupus having the major features of keratinocyte damage and mononuclear cell infiltrate. Skin lesions often present at a few weeks of life, but may be present at birth. Spontaneous resolution within weeks or months without permanent residua is the expected outcome. Affected individuals tend to be healthy later in childhood. There does however appear to be an increased risk for children who have had NLE to develop autoimmune diseases later in childhood or adulthood such as juvenile rheumatoid arthritis, Hashimoto thyroiditis and diabetes mellitus.
At present, practices and opinions differ regarding recommendations for prophylactically treating anti-Ro positive women during pregnancy. What is generally agreed on is that if systemic corticosteroids are given, dexamethasone or betamethasone are better choices than prednisone or prednisolone, as they are not inactivated by placental enzymes and so reach the fetal circulation largely intact.
It is quite often the case that autoimmunity in the mother is not detected until the birth of her first child with NLE. Several studies indicate that, with time, the mothers who were initially asymptomatic eventually develop signs and symptoms of autoimmunity themselves, in particular Sjögren syndrome, systemic lupus erythematosus and undifferentiated connective tissue disease.
Download images for this case
Treatment
Initial treatment was packed red blood cells & platelet transfusions for the pancytopaenia. He was then given intravenous immunoglobulin (IVIG) to create a dilutional effect and high pulse dose pulse of methylprednisolone and oral prednisone.
The seizures were treated with phenobarbitone.
Gradually the cytopaenias responded to therapy with resolution of the anaemia and normalisation of platelet count.
Post transfusion and glucocorticoid blood smears showed resolution of fragments and spherocytes.
Discharge blood results:
- Hb:11,8
- MCV: 79,5
- Platelets: 181
- Neutrophil: 3.8
- Anti Ro: 18
- Anti La: negative
Note: There are no established guidelines or consensus for effective treatment and management of this haematologic disease.
General recommendations are to try combinations or isolated forms of the following:
- Glucococorticoids
- IVIG
- Plasmapharesis
- Plasma exchange
Download images for this case
Final outcome
The child continues to improve and is anticipated to make a full recovery.
Download images for this case
References
1. C McGeachy et al (2009). Anti-RNP neonatal lupus in a female newborn. Lupus; 18; 172-174
2. R Klauninger et al (2009). Serologic follow-up of children born to mothers with Ro/SSA autoantibodies. Lupus; 18; 792-798
3. Lela A. Lee. (2009) The clinical spectrum of neonatal lupus. Archives of Dermatological Research. 301:107-110
Download images for this case
Evaluation – Questions & answers
What is the diagnosis?
Which autoantibodies are associated with NLE?
What is the mechanism of disease?
Which organ systems are affected?
What are the long term consequences of NLE on the affected infant?
There also appears to be an increased risk for development of autoimmune diseases later in childhood or adulthood.
What causes anaemia, thrombocytopaenia and occasionally pancytopaenia in NLE?
What investigations can be carried out to assess pancytopaenia?
- FBC
- Bone marrow trephine biopsy
- LDH where a high reading indicates general cell destruction
- Haptoglobin which decreases when consumed by high release of haemoglobin
- Coombs test which identifies anti-red cell antibodies in plasma – i.e. proof of circulating anti-red cell antibodies
Download images for this case
Multiple Choice Questions
Earn 1 HPCSA or 0.25 SACNASP CPD Points – Online Quiz.
Download images for this case