- Patient presentation
- History
- Differential Diagnosis
- Examination
- Investigations
- Discussion
- Treatment
- Final Outcome
- Evaluation – Questions & answers
- MCQ
- References
Patient presentation
A four year old boy presents with fever, abdominal pain with abdominal guarding and difficulty breathing. He also complains of headaches and frequent skin abscesses which take a long time to heal.
Acknowledgement
This case study was kindly provided by Dr Monika Esser MMed Paed, Head of Division of Immunology, N.H.L.S Coastal Branch, Tygerberg Hospital.
History
His perinatal course was uneventful; he was breastfed for 6 months and tolerated all childhood vaccinations well. He had uncomplicated chickenpox at age 2 years.
He does have a history of failing to thrive, measuring below the 3rd centile for height and weight.
Throughout his childhood he has suffered from frequent abscesses and delayed healing has been noted.
At age 3 he presented to hospital with pyrexia, a swollen right knee and a poorly healed superficial abscess on his left foot. He was admitted to the surgical ward for arthrotomy of the knee and debridement of the foot. All other systems were normal on investigation.
Staphylococcus aureus was isolated from the knee and histology of the foot lesion showed granulomas. Full Blood Count revealed a hypochromic microcytic anaemia; CRP was 200 and ESR 90. Serum immunoglobulin’s all tested normal.
The patient was treated with a full course of Clindamycin and a one week course of nasal mupirocin administered at home. The parents were also instructed on hygiene measures to prevent future impetigo and boils e.g. having own face cloth, washing with Hexachlorophene, hair washing with Povidone/Iodine twice per week, hot wash for underwear, keeping nails short, etc.. The family pet was also investigated for Staphylococcal lesions.
Family and Social History
- He is an only child with two healthy parents.
- An uncle on his maternal side died in his teens from recurrent infections.
- Social circumstances are adequate with running water and toilet facilities inside the house.
- There is one family pet.
Differential Diagnosis
- Malnutrition – failing to thrive, iron deficiency anaemia
- Lack of hygiene e.g. scabies and neglected impetigo, lack of health education of parents, and possible lack of access to healthcare
- Eczema as a precipitating factor, rapidly colonised with Staph aureus.
- HIV
- Complement disorder
- Chronic Granulomatous Disease (CGD)
Examination
On examination the following was found:
- The child was pyrexial
- Marked guarding and tenderness of the abdomen.
- Decreased air entry into the right lower lobe.
- Mild jaundice
- Multiple scars on the skin from healed abscesses are noted.
- Patient does not appear acutely ill.
Investigations
On abdominal ultrasound loculated fluid is seen in the right hepatic lobe and right lower lung region with communication through the diaphragm.
On laparotomy and thoracotomy purulent material is drained and Streptococcus milleri is cultured.
Discussion
The surgeon requested additional consults from the Microbiologist, the Clinical Immunologist and social worker for further evaluation as he suspects an Immune Deficit.
The Microbiologist confirms a sensitive organism but also recommends extended fungal and anaerobe culture. He alerts to the possibility of S.milleri spread to the brain– but CT Brain is normal.The Immunologist emphasises that an immunocompromised/deficient patient may not present with the typical clinical signs of infection and recommends a total complement assay and a neutrophil function test – the nitroblue tetrazolium (NBT) test.
The NBT test
The nitroblue tetrazolium (NBT) test: activated neutrophils are tested for their ability to phagocytose and reduce NBT.
The results are seen here:
(a) Control shows reduced NBT seen as dark-blue crystals in the neutrophils.
(b) Patient sample of stimulated neutrophils shows the patient fails to reduce NBT. The patient has an NBT result of zero (0) compared to the adult control.
Download images for this case
Treatment
Patient was treated with Trimethoprim/Sulphamethoxazole and antifungal prophylaxis.
A drug company also donated gamma interferon, which is used to normalise the oxidative burst of neutrophils to most organisms but is not effective for treating fungal infections.
The parents were again educated about practicing careful hygiene measures.
Download images for this case
Final Outcome
At age 20, now a college student, despite treatment and excellent compliance the patient has had a recurrence of liver abscesses. He has also recently been suffering from severe acne.
Despite Immunokine treatment and antimicrobial prophylaxis, he is still immunodeficient.
Possible reasons:
- Non compliance- teenage rebellion
- The drug may be inactive – old stock (donation)
- Skin abscesses (Acne) may have been neglected – poor hygiene
- Limited access to health care – self-sufficient adult now, no transport or money.
- Lack of education of the patient
- Delay in presentation – peripheral hospital not fully aware of his Immunodeficiency.
Download images for this case
Evaluation – Questions & answers
What is the diagnosis?
Why was the nitroblue tetrazolium (NBT) test performed?
The NBT test is one of the best ways to confirm Chronic Granulomatous Disease i.e. polymorphs demonstrate an inability to reduce NBT. It is also useful for detecting carrier state, looking at the blood from carriers of CGD will contain a mixture of normal and abnormal neutrophils (Nathan et al., 1969).
This patient has an NBT result of zero (0) compared to the adult control. Which organisms is he susceptible to?
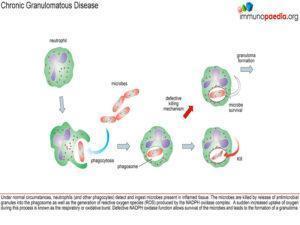
Patients with CGD are susceptible to severe and recurrent infections due to catalase-positive organisms and organisms resistant to nonoxidative killing. These microorganisms produce catalase that breaks down endogenously produced hydrogen peroxide; the generation of oxygen radicals by a normally functioning phox system is needed to ensure the death of the infecting microorganisms. These organisms include S.aureus, Burkholderia cepacia and enteric bacteria, particularly Serratia marcesens. Fungal infections, such as Aspergillus spp are also common, making up 20% of infections.
Explain why he would not be unduly susceptible to Strep pneumonia infections
Streptococcus pneumoniae, does not produce catalase, having the capacity to generate its own hydrogen peroxide, and is thus far less resistant to intracellular killing than microorganisms that are catalase producers.
Which part of the immune system is affected?
CGD is a primary immunodeficiency that affects phagocytes of the innate immune system.
Why would a B Cell-related cause be unlikely?
The serum immunoglobulins are normal and the patient has had no respiratory infections.
Why would a T cell-related deficit be unlikely?
Due to the patient’s adequate response to live vaccines and viral infection.
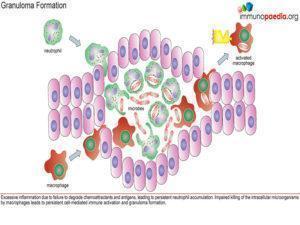
Why is there granuloma formation?
When CGD patients become infected they often have extensive inflammatory reactions. The excessive inflammation is thought to be due to failure to degrade chemoattractant and antigens, leading to persistent neutrophil accumulation. Impaired killing of the intracellular microorganisms by macrophages may lead to persistent cell- mediated immune activation and granuloma formation. Granulomas will typically develop in the skin, gastrointestinal tract (GI) and genitourinary tract (GU). At diagnosis, some patients present with symptoms related to these granulomas. Symptoms of GI granulomas include dysphagia, nausea, vomiting, abdominal pain, and obstruction and symptoms of GU obstruction include dysuria, incontinence, abdominal discomfort, and urinary retention(Pagán & Ramakrishnan, 2018; Prieto-Bermejo et al., 2021).
What is the treatment?
Management of chronic granulomatous disease revolves around two goals:
- Early diagnosis so that antibiotics can be given to prevent infections, and
- Educating the patient and care givers about the condition so that prompt treatment can be given if an infection occurs.
Typically trimethoprim/sulfamethoxazole is prescribed to prevent bacterial infections. Fungal infection is commonly prevented with itraconazole. Interferon, is also prescribed for the prevention of infection in CGD. It has been shown to prevent infections in CGD patients by 70% and to reduce the severity of infections. It has the ability to give CGD patients more immune function and therefore greater ability to fight off infections. Gene therapy is currently being studied as a possible treatment. CGD is well-suited for gene therapy because it is caused by a mutation in single gene which only affects one body system (the hematopoietic system).
Download images for this case
Multiple Choice Questions
Earn 1 HPCSA or 0.25 SACNASP CPD Points – Online Quiz
Download images for this case
- Gennery, A. R. (2021). Progress in treating chronic granulomatous disease. British Journal of Haematology, 192(2), 251–264. https://doi.org/10.1111/BJH.16939
- Nathan, D. G., Baehner, R. L., & Weaver, D. K. (1969). Failure of nitro blue tetrazolium reduction in the phagocytic vacuoles of leukocytes in chronic granulomatous disease. The Journal of Clinical Investigation, 48(10), 1895–1904. https://doi.org/10.1172/JCI106156
- Pagán, A. J., & Ramakrishnan, L. (2018). The Formation and Function of Granulomas. Annual Review of Immunology, 36, 639–665. https://doi.org/10.1146/ANNUREV-IMMUNOL-032712-100022
- Prieto-Bermejo, R., Romo-González, M., Pérez-Fernández, A., García-Macías, M. C., Sánchez-Bernal, C., García-Tuñón, I., Sánchez-Yagüe, J., Sánchez-Martín, M., & Hernández-Hernández, Á. (2021). Granuloma Formation in a Cyba-Deficient Model of Chronic Granulomatous Disease Is Associated with Myeloid Hyperplasia and the Exhaustion of B-Cell Lineage. International Journal of Molecular Sciences, 22(16). https://doi.org/10.3390/IJMS22168701
- Yang, A. H., Sullivan, B., Zerbe, C. S., De Ravin, S. S., Blakely, A. M., Quezado, M. M., Marciano, B. E., Marko, J., Ling, A., Kleiner, D. E., Gallin, J. I., Malech, H. L., Holland, S. M., & Heller, T. (2023). Gastrointestinal and Hepatic Manifestations of Chronic Granulomatous Disease. The Journal of Allergy and Clinical Immunology: In Practice, 11(5), 1401–1416. https://doi.org/10.1016/J.JAIP.2022.12.039
- Yu, H. H., Yang, Y. H., & Chiang, B. L. (2021). Chronic Granulomatous Disease: a Comprehensive Review. Clinical Reviews in Allergy & Immunology, 61(2), 101–113. https://doi.org/10.1007/S12016-020-08800-X