A ground-breaking study published in the European Journal of Obstetrics and Gynaecology examines the factors that influence contraceptive preferences among postpartum women in Brazil. The research was conducted at a large public maternity hospital in Fortaleza, Brazil, and involved 294 women interviewed within 48 hours after giving birth. The study aimed to assess the women’s immediate contraceptive preferences and whether they were using their desired method six months postpartum. The results highlight the importance of offering postpartum contraceptive services and the impact of social and demographic factors on contraceptive choices.
Further readings: Cyto2018 Highlight: Immune Clock of Pregnancy
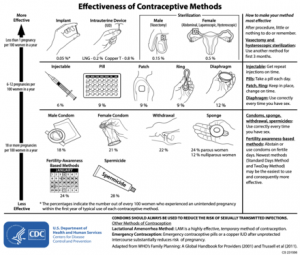
The study found that the majority of women (39.1%) preferred intrauterine devices (IUDs) as their contraceptive method, followed by implants (33%) and injectable hormonal contraceptives (17%). These methods are considered long-acting reversible contraception (LARC) and are favoured for their high efficacy and low maintenance. The preference for LARC methods is significant, as these options provide prolonged protection without the need for daily adherence, which is often a challenge for new mothers. Only a small percentage (6.1%) preferred contraceptive pills, and an even smaller group opted for sterilization or condoms.
One of the key findings was that only 42.5% of the women were using their desired contraceptive method six months postpartum. Adolescents, who made up 56.5% of the sample, were more likely to be using their desired contraceptive method compared to adults. Among adolescents, 54.8% adhered to their chosen method, while only 26.6% of adults were using their preferred method six months after childbirth. This disparity suggests that younger women may be more open to contraception or face fewer barriers to access.
The research identified several factors that contributed to whether or not women were using their chosen contraceptive method six months after childbirth. One of the most significant factors was whether the woman had initiated contraception before hospital discharge. Women who started contraception immediately after giving birth were 4.61 times more likely to be using their desired method six months later. This finding underscores the importance of providing immediate postpartum contraception in healthcare settings, as the window for effective contraceptive counselling and initiation is often limited.
The study also found that race and age played a role in contraceptive adherence. White women were more likely to use their desired method than women of other racial backgrounds, and younger women were more likely to adhere to their contraceptive plan than older women. This suggests that socio-economic factors and cultural attitudes towards contraception may influence access and adherence.
Access to contraceptives was a recurring issue. Many women who did not use their chosen method cited difficulty obtaining the contraceptive as a primary reason. This issue is particularly acute in regions with limited healthcare infrastructure, highlighting the need for policies that ensure easy and affordable access to contraception for all women, especially in the postpartum period. The study advocates for the inclusion of contraceptive counselling in prenatal care programs and stresses the importance of providing free or low-cost contraceptives to ensure that women can use their preferred methods.
Overall, this study highlights the critical role of healthcare providers in facilitating postpartum contraception and the need for policies that improve access to long-acting reversible contraceptives. It emphasizes the importance of early contraceptive counselling and initiation, particularly in low-resource settings where follow-up care may be limited.
Journal Article: Meireles Castro Maia, Elaine, et al. “Choice and Factors Associated to the Use of Contraceptive Methods among Postpartum Women: A Prospective Cohort Study.” European Journal of Obstetrics & Gynecology and Reproductive Biology, vol. 298, 29 Apr. 2024, pp. 1–5, www.sciencedirect.com/science/article/abs/pii/S0301211524002136, https://doi.org/10.1016/j.ejogrb.2024.04.038.
Summary by Faith Oluwamakinde