Preterm birth, defined as delivery before 37 weeks of gestation, remains a significant cause of neonatal morbidity and mortality worldwide. Spontaneous preterm birth (sPTB), which accounts for a considerable portion of these cases, presents a challenge in obstetric care due to its unpredictable nature and unclear etiology. Recent research has focused on identifying non-invasive markers that could predict preterm labour, and plasma biomarkers have emerged as promising candidates.
Read further: Preterm births alter ATP production and immunity and Functional B cells needed to prevent preterm birth
A recent study explored the utility of specific plasma biomarkers in predicting spontaneous preterm birth. These biomarkers were evaluated in a cohort of pregnant women, comparing those who experienced spontaneous preterm birth to those with term deliveries. The study highlighted several biomarkers involved in inflammation and immune regulation that were significantly elevated in the sPTB group, providing insights into the underlying mechanisms of preterm labour.
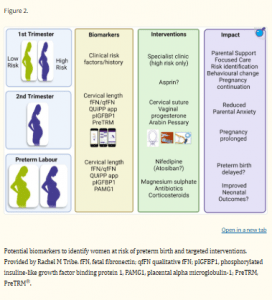
Figure 1: Potential biomarkers to identify women at risk of preterm birth and targeted interventions. Provided by Rachel M Tribe. fFN, fetal fibronectin; qfFN qualitative fFN; pIGFBP1, phosphorylated insuline-like growth factor binding protein 1, PAMG1, placental alpha microglobulin-1; PreTRM, PreTRM®.
Inflammatory markers, such as cytokines and chemokines, were found to play a critical role in triggering the preterm birth process. These biomarkers are involved in the inflammatory cascade that precedes the initiation of labour. By identifying elevated levels of these markers in maternal plasma, clinicians may be able to detect women at higher risk for preterm birth earlier in their pregnancy. This would allow for closer monitoring and the potential to implement interventions aimed at prolonging pregnancy and improving neonatal outcomes.
The study also underscores the importance of developing a multi-marker panel to increase the predictive accuracy of plasma biomarkers. While individual markers show promise, combining several biomarkers could improve sensitivity and specificity, making this approach more practical for clinical use. The authors of the study emphasize that while the current findings are promising, further research is needed to validate the utility of plasma biomarkers in larger, more diverse populations.
The potential impact of plasma biomarkers in the clinical setting is significant. A reliable, non-invasive test could revolutionize the management of preterm birth by allowing healthcare providers to stratify patients based on their risk of sPTB, providing personalized care and potentially reducing the incidence of preterm-related complications.
Journal article: Gravett MG, Menon R, Tribe RM, Hezelgrave NL, Kacerovsky M, Soma-Pillay P, Jacobsson B, McElrath TF. Assessment of current biomarkers and interventions to identify and treat women at risk of preterm birth. Front Med. 2024;11:1414428. doi: 10.3389/fmed.2024.1414428.
Summary by Faith Oluwamakinde










