This week we highlight the last SAIS/Immunopaedia webinar by Professor Theresa Rossouw, Dr Sanjay Lala and Dr Asma Salloo.
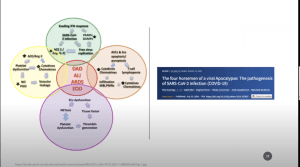
Schema representing the most remarkable pathophysiological events involved in each of the four vicious feedback loops and the complex interactions established between them. Intersections between circles represent interaction between loops. The central circle colored in red means the final events of the physiopathologic cascade. The vicious viral loop is depicted in green, the hyperinflammatory loop is colored in orange, the ACE2/Ang-(1–7) loop is colored in yellow, and the hypercoagulation loop is colored in purple. IFN = interferon; PAMPs = Pathogen-associated molecular patterns; DAMPs = Damage-associated molecular patterns; SARS-CoV-2 = Severe acute respiratory syndrome Coronavirus 2; AECs = Alveolar epithelial cells; ECs = Endothelial cells; ACE2 = Angiotensin-converting enzyme 2; Ang-(1–7) = Angiotensin 1–7; ACE = Angiotensin-converting enzyme; Ang II = Angiotensin II; NO = Nitric oxide; PGI2 = Prostacyclin; MΦ = Macrophages; PMNs = Polymorphonuclear neutrophils; DAD = Diffuse alveolar damage; ALI = Acute lung injury; ARDS = Adult respiratory distress syndrome; EOD = End-organ disease.
Prof Rossouw is a clinician-scientist who holds PhDs in immunology and philosophy based at the University of Pretoria. Her talk during the webinar focused on “Immunological pathways leading to a COVID-19 cytokine storm”. Cytokine storm is an acute systemic inflammatory syndrome due to hyperactive immune response which leads to a release of IFNs, interleukins, TNF and other mediators that activate innates cells and results in fever in multiple organ failure (See image). Cytokine storm is a blanket term used to describe multiple pathologies including cytokine release syndrome, macrophage activated syndrome, sepsis, acute respiratory distress syndrome (ARDS) and many other. She highlighted conflicting studies that dispute the existence of COVID-19 associated cytokine storm, where cytokine profile associated with hyperinflammation in severe COVID-19 patents also includes upregulation of other cytokines IL-10, and chemokines IP-10 and MCP-1, markers not always associated with cytokine storm. She then described a “simplistic hypothesis” where severe COVID-19 is associated with a pro-inflammatory cascade leading to hyperactive Th1/Th17 cells, vascular leakage and lung damage, while a sufficient anti-inflammatory response in mild SARS-CoV-2 sufficiently controls pro-inflammatory responses. This hypothesis could be the reason for mild disease in children and pregnant women, as they have a skewed Th2, anti-inflammatory response. Further, she described that the spectrum of COVID-19 is likely as a result of 4 pathophysiological pathways: viral immunity, hyperinflammation, AE2/Ang-(1–7) pathway and the hypercoagulation. Read our articles on COVID-19 & Cytokine storm
- Cytokine Release Syndrome & COVID-19
- Can the Cytokine Release Syndrome in COVID-19 patients be treated using CCR5 blocking antibody therapy?
- COVID-19 – Cytokine storm syndromes and immunosuppression
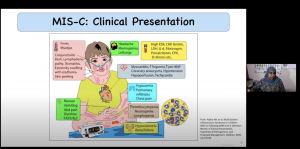
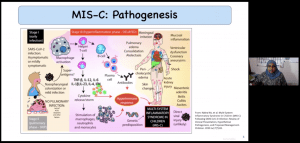
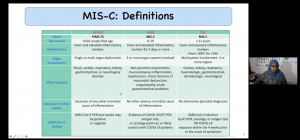 Dr Salloo is a paediatric-intensivist based at the Chris Hani Baragwanath Academic Hospital (CHBAH) in Johannesburg, one of her research focuses is on multisystem inflammatory syndrome in children (MIS-C). Her talk focused on “Clinical manifestations of COVID-19 in children”. She highlighted that children (< 10 hours) have a lower susceptibility to infection and development of severe COVID-19. At CHBAH as of 10 October, 130 COVID-PCR+ children (<15 years) were admitted, 12 of whom required ICU with varying levels of COVID-19 pathologies including 2 MIS-C, 4 COVID-pneumonia & 1 ARDS. During the early stages of pandemic multiple reports of SARS-CoV-2 associated multi-organ inflammation and hyperinflammatory shock were reported, most notably was an increase in reports of Kawasaki like diseases in older children. She ended her talk giving a brief overview of:
Dr Salloo is a paediatric-intensivist based at the Chris Hani Baragwanath Academic Hospital (CHBAH) in Johannesburg, one of her research focuses is on multisystem inflammatory syndrome in children (MIS-C). Her talk focused on “Clinical manifestations of COVID-19 in children”. She highlighted that children (< 10 hours) have a lower susceptibility to infection and development of severe COVID-19. At CHBAH as of 10 October, 130 COVID-PCR+ children (<15 years) were admitted, 12 of whom required ICU with varying levels of COVID-19 pathologies including 2 MIS-C, 4 COVID-pneumonia & 1 ARDS. During the early stages of pandemic multiple reports of SARS-CoV-2 associated multi-organ inflammation and hyperinflammatory shock were reported, most notably was an increase in reports of Kawasaki like diseases in older children. She ended her talk giving a brief overview of:
- The different definitions of COVID-19 associated MIS-C (see table)
- Immunopathogenesis of MIS-C
- MIS-C clinical presentation
- Management of MIS-C
Read previous articles on Paediatric COVID-19
- SARS-CoV-2 infection in young children and Kawasaki-like disease.
- The different clinical characteristics of COVID-19 between children and adults.
- Why is COVID-19 so mild in children?
Summary by Cheleka Mpande