For the second webinar of the International Union of Immunological Societies (IUIS) webinar series in collaboration with Immunopaedia and Frontiers Immunology, we were treated by an amazing talk from Professor Akiko Iwasaki titled – Immune responses to SARS-CoV-2.
Akiko Iwasaki, PhD, is the Sterling Professor of Immunobiology and Molecular, Cellular, and Developmental Biology at Yale University, and Investigator of Howard Hughes Medical Institute. She received her PhD from University of Toronto in Canada and her postdoctoral training from National Institutes of Health. Her research focuses on mechanisms of immune defence against viruses at the mucosal surfaces. She is Lead Investigator of the Yale COVID-19 Recovery Study, which aims to determine the changes in immune response of people with long COVID after vaccination. Dr. Iwasaki also leads multiple other studies to interrogate the pathobiology of long COVID.
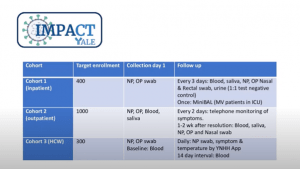
Prof. Iwasaki began her talk with a brief overview of some brilliant findings made by her and her group in addition to gaps they are looking to fill with further research. Firstly, they were able to establish and recruit from a biobank of patients meeting certain criteria for SARS-CoV-2 infection, collecting nasopharyngeal (NP) and oral swabs as well as blood and saliva (Figure 1).
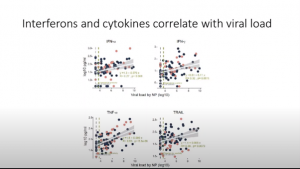
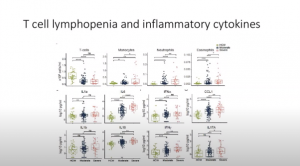
Following on from this, (IMPACT Yale study), they were able to develop a longitudinal immune phenotype in COVID-19 patients. They found (Figure 2), that circulating T cell numbers dropped in level in both moderate and severe patients with no accumulation in organs with an increase in monocytes, neutrophil, and eosinophil numbers in severe patients, in conjunction with an increase in inflammatory chemokines and cytokines. They were also able to show that specific cytokines positively correlate with viral load which is seen to increase in NP swabs in severe patients (Figure 3).
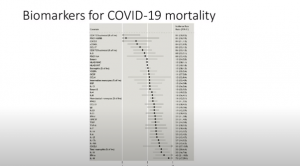
They also validated that the virus can evade specific immune response mechanisms such as the interferon response. Her team were able to characterise and identify biomarkers for COVID-19 mortality (Figure 4), additionally being able to distinguish patients who recover vs. patients who go on to develop worse disease. It was interesting to see how people with severe COVID had a delayed antibody production time course and had a higher production of anti-spike and anti-RBD antibodies. This allowing the grouping of patients from mild to severe disease phenotype.
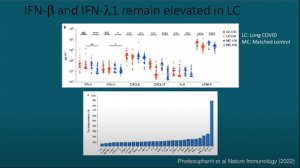
Following their investigations on acute COVID infection, they have started focusing on, as Prof. Akiko termed, a “parallel pandemic,” i.e., long covid. She highlighted that there are three paths to long COVID (Figure 5). It is known that long COVID causes lasting symptoms involving multiple organs. She also showed data illustrating how specific interferons remain elevated in long COVID patients (Figure 6). It was interesting to see that her group and others developed a model used to investigate how infection of the lung with COVID (mild infection), may lead to significant long-term CNS effects.
In closing, Prof. Iwasaki ended off highlighting new avenues of research that her team and collaborators are pursuing, stating that they are now aiming to understand immunological and physiological determinants of disease pathogenesis of long COVID to inform rational diagnosis and therapy.
Watch the fascinating talk below
Summary by Stefan Botha